Black Family Health
February 7, 2023

When
February 7, 2023
5:30 p.m. - 7:30 p.m.
Where
Virginia Tech Carilion School of Medicine
2 Riverside Circle, Roanoke, VA 24016
Auditorium M203
Contact
Karyna Nevarez at karynad@vt.edu
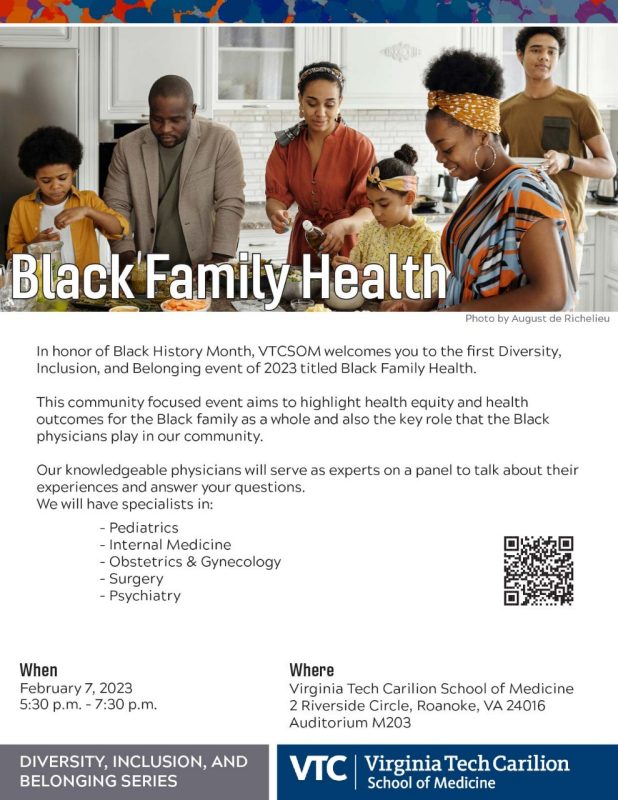
In honor of Black History Month, VTCSOM welcomes you to the first Diversity, Inclusion, and Belonging event of 2023 titled Black Family Health.
This community focused event aims to highlight health equity and health outcomes for the Black family as a whole and also the key role that the Black physicians play in our community.
Our knowledgeable physicians, with experience in the following specialties will serve as experts on a panel to talk about their experiences and answer your questions:
- Pediatrics
- Internal Medicine
- Infectious Diseases
- Obstetrics and Gynecology
- Family Medicine
- Surgery, and
- Psychiatry
Speakers
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
Video Transcript
Dr. Kemi Bankole
We're ready to go? All right. Well, thank you everyone that's been able to make it here in person, and for everyone that is on Zoom. I am Dr. Kemi Bankole, I'm a geriatric psychiatrist here at Carilion Clinic, and the chief diversity officer at the medical school. This diversity inclusion belonging series is a part of the work that we do with and for our community, and it is sort of broaching different topics that are important to us and that we feel are important to our community as well. So this particular DIBS, diversity, inclusion and belonging series, is on Black family health. And I'm here to introduce or actually have our panelists introduce themselves. A group of well-accomplished Black clinicians and physicians who practice here in our community. So first of all, thank you all for making time out of your busy practices to be here. And so we'll start off by going round with introductions. Do you want to start? >> Hi, good evening. Can you hear me? >> Yes, we can hear you.
[1:32] Introductions
[Dr. Ayesha Kelly]>> My name is Dr. Ayesha Kelly, I'm a general surgeon who works in Lexington, Virginia. So about 45 min away from here. And we do bread and butter general surgery, Rockbridge Community Hospital, which is a Carilion facility.
[Alyssa “Brooke” Watkins]>> Hello everybody. My name is Dr. Alyssa, I go with middle name, Brooke Watkins. I am an OBGYN here at Carilion. I'm a newer faculty, been here about a year and a half. But I work out of Riverside, and at the hospital in labor and delivery, and in the ORs as well.
[Dr. Oluyemisi Solomon]>> Hi everyone, I'm Oluyemisi Solomon. I trained here in Roanoke up with Carilion Family Medicine, and I practice in Rocky Mount, about 30 five-ish minutes from here, depending on traffic. And I'm Jack of all trades.
[Dr. Olivia Asamoa]>> Hello everybody. My name is Dr. Olivia Asamoa, I am with the department of pediatrics. I also trained here at Carilion, and just finished residency last year, so I'm newer into the practice. And I practice out of our new building in Tanglewood, on Electric Avenue.
[Dr. Sharon Williams]>> Hello everyone. I am Dr. Sharon Williams, I'm one of the general surgeons here. I've been here about five years, and I am trained in minimally invasive and general surgery. So I do some robotic surgery, but also just the basic general surgery.
[Dr. Kimberly Clay] >> Hello. Good afternoon, everybody. I'm Dr. Kimberly Clay, I'm an endocrinologist here at Carilion Clinic. I work at the Riverside 3, not too far from here. We do general endocrinology there. So I do a lot of thyroid, diabetes, osteoporosis. One of my specialties is doing thyroid biopsies. So glad to be here.
[Dr. Kemi Bankole]>> Dr. Baffoe-Bonnie do you want to introduce yourself?
[Dr. Anthony Baffoe-Bonnie]>> Sorry. I got caught up in a couple of things. My name is Dr. Anthony Baffoe-Bonnie. I'm an infectious disease physician and hospital epidemiologist.
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[4:02]: What are some of the challenges you face in your day-to-day practice?
[Dr. Kemi Bankole]>> That's our illustrious panel for this evening. We're going to start off asking panelists questions and then towards the end we'll take some questions from both our live audience and our virtual audience. My first question to our panelists are, what are some of the challenges you face in your day-to-day practice that you'd want folks to know about?
[Dr. Oluyemisi Solomon]>> I'm family practice. I would say the biggest challenge for me is time constraints. Like I said before, I'm jack of all trades. I'm given very little time. I see over 20 patients a day. My patients like to come in with a list of problems of which they went every single one addressed. Whether it's COPD, diabetes, hypertension, or they stubbed their toe and now that hurts or is infected, or they need a Pap smear as well all in that same visit. It's really hard to do. With the time constraint, I'm trying to do it all in one appointment. Then of course, I'm running behind and they get upset in the waiting room. It's just that really backlog, the time constraints just asks us to do.
[Dr. Kemi Bankole]>> We really need to overhaul the whole healthcare system so we can make sure that our family physicians and all our other doctors have enough time to see our patients.
[Dr. Oluyemisi Solomon]>> That would be helpful. You guys see my special colleagues who know what complaint? Several times my patients will say, [inaudible] actually. They would say, I saw my heart doctor and he would only address my heart and not my cold, not my aching foot, and my aching knee, and this and that.
[Dr. Ayesha Kelly]>> I totally agree with that. Even for us, I'm a general surgeon in a rural facility and we don't have dermatology, we don't have cardiology on a regular basis. We don t have nephrology, we don't have pulmonology. For me in my practice, probably the biggest challenge is getting people to the appropriate specialist or their PCP when they want everything addressed by the general surgeon who is not going to be able to solve your chronic nausea that you woke up with and you go to bed with. Or your skin lesion that has been growing for the last year and is now invaded into your nose and we need a dermatologist with moles and all those things. Getting people from Lexington to whatever tertiary care center and meeting the needs of those patients is probably the biggest challenge, especially since COVID.
[Dr. Kemi Bankole]>> Thank you.
[Dr. Brooke Watkins]>> I would have to echo bothpeople prior to me and adding that I think too, one of the biggest challenges for me is that it's in access to care issue because Carilion along with LewisGale Physician to women, are one of the only OB-GYN practices that are, there's a lot of the surrounding cities that have closed for now obstetric and OB-GYN practices like Martinsville. Also we're like a OB-GYN desert at this point. We have a lot of patients that come to see us from outside communities. Then a lot of these patients also too, specifically a lot of the minority patients, they don't have PCPs and so they use us as their PCP. They're, as well, I'm pregnant, but, I also have this. I'm like, okay, great. Let's see about the pregnancy first [LAUGHTER] or they're coming from the annual and the annual turns into this long drawn out problem visit, which is fine. I'm happy to do it. But again, time restraints, we're seeing so many complex patients and patients from far away, so I'm trying to get them all that they need in that one visit so that they don't have to travel two hours for another just short visit is hard along with the MyChart messages and the patient calls. It's time really. [LAUGHTER]
[Dr. Olivia Asamoa]>> Again, I think I would echo that as well. Because seeing children and you are saying between 20 and 30 in a day and they all come in screaming and crying and the parents will coming with a list and try and address every single problem on that list. I think another big one is just resources, just knowing what resources are available. Because parents come in and they're coming to see a dentist while they're on Medicaid. Most of the places that take Medicaid closed during the pandemic. Trying to get them into Carilion Dentistry who has a backlog of patients, it's just always a lot. I think trying to identify resources for your patients, particularly the ones who are coming two hours, because some of our patients are driving two hours or coming from Martinsville or Danville just to see us because there's nothing out there for them. It's just a struggle on a daily basis trying to get people to the right people in a timely fashion because that's always another thing if they don't understand that not everything can happen on their timeline.
[Dr. Anthony Baffoe-Bonnie]>> I'll add to the resources and knowledge about resources. It's really important. I do a lot of HIV work and also work on men who have sex with men and who would benefit from pre-exposure prophylaxis. It's unfortunate that sometimes you will see an HIV patient, a young person who is HIV positive and they did not know that there were PrEP medications that they could avail themselves to. That's one big challenge that we have to solve as a community and as a system, as a society we could do better sharing such information. That's one. Then two, when we have HIV patients, there's this thing called the Ryan White grant, which essentially I tell most of my patients you've got to try hard to die from HIV in the US. You really have to try hard because these things are free and the medicines work. Patients with HIV will live as long as anybody without HIV. But some people don't know about that. By the time they seeing me, they're not doing well, and that is a challenge that I hope we can overcome.
[Dr. Sharon Williams]>> I can echo some of that though for us here in Roanoke, who are doing general surgery. We're having a time constraint that's almost the opposite of what a lot of you guys are talking about in that we're having a shortage of OR time. I'm available and I could come and operate, but we don't have the ORs available because we don't have enough anesthesiologists right now. Our whole system is working on it, they're going to get a residency for anesthesia. They're opening a CRNA school, all this stuff. But right here today people are waiting six months for some basic surgeries like hemorrhoids surgery and stuff like that. People are actually suffering but it's not going to kill them. It's hard for them to be patient. I've been dealing with that for the past almost a year and that's been a struggle.
[Dr. Kimberly Clay]>> Like everyone else said, [LAUGHTER] I feel like going on and on. But I think one thing I would like to add specially for us, nursing support has really been a big issue for us. The education that we have to provide for particularly our diabetics, pumps, meters, diet, things like that. We have constraints with actually some of our dietitians availability, nursing availability to be able to instruct the patients on how to use some of the technology. Then of course, access like you guys, we have folks from Martinsville. I had someone came yesterday from West Virginia. We have people from Tennessee, especially down to Southern Virginia there's no endocrinology groups. Pretty much if you're Blacksburg to Martinsville and up and even like I said, sometimes other states they end up coming to see us. Not having enough time as always, because like you said, I wish it was always one problem because of diabetes alone. You're talking about blood pressure, cholesterol, blood sugars, and then of course we do osteoporosis, thyroid and don't be surprised, I get the foot toe question myself. I'm like, I don't think you want me to try to look at that, I'll be honest with you. We're on the same challenges everyone else has here.
[Dr. Kemi Bankole]>> Thank you all for that. You brought up a lot of systemic issues with how we are being a trauma one level of care hospital in an area that's surrounded by a very rural population and bringing the challenges that having this space. It's not like we have two, three, four level one trauma hospitals here. [LAUGHTER] Thank you all for that. You've talked about challenges that you face.
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
[Dr. Kimberly Clay]>> I'll start probably like a lot of people financial, so insurance coverages, that's the biggest thing. And obviously it changes year to year, but folks who could get a Dexcom last year can't get it this year. Who could get a Freestyle Libre, both of which are continuous glucose monitoring. So they don't have to prick their fingerstick, which everybody doesn't want to do that. I haven't met too many who liked that one. But that's a big thing for us as insurance coverage, being able to come see us because of lack of insurance. Getting the studies that we need thyroid ultrasound, procedures, just that's the biggest issue that I think most of my patients seem to have.
[Dr. Brooke Watkins]>> I would echo that 100%. I've had more battles with insurance than I've had in my life this past year. And I don't necessarily know why, but I think insurance is a huge barrier for a lot of patients, especially when things that we do are very expensive. And so patients need surgery but can't have surgery because they don't have insurance. They have to apply for charity care and then it takes forever and then our ORs are backed up, so then they're waiting six months to get a hysterectomy for bleeding that they've been bleeding for a long time. The access to care issue and just resources in general I think is the biggest barrier. And then a lot of times too, with having to travel so far, it's hard to get everything scheduled right now because scheduling is so backed up because we have so many patients that need everything. And so scheduling for patients as well it's hard for a lot of patients who don't have insurance they rely on their jobs, they have to travel, but they can't get off because they need their job. So it's just a cycle of not good access to care.
[Dr. Sharon Williams]>> I see the same thing for I do a lot of hernia repairs and the patients they can't afford to take the time off even if their insurance will cover certain things. If I tell him they have to be out for a couple of weeks because I'm doing a primary repair or something. That's a struggle for them or their disability only covers like two-thirds and that's not enough to pay the bills. So they have to delay and I’ll sometimes see people again a year-and-a-half later and they saved up enough money, so now they can or they got better insurance that covers more or something, so I see that as well.
[Dr. Ayesha Kelly]>> Not to add to everybody's but for my area, a lot we'd have a lot better access if patients were educated better. In my community we have a big problem with patient education. We have a big gap between those who are educated and those who are not educated. And those who are not educated, I have some patients who still have outhouses. I still have some patients who don't have hot water. I have some patients who don't read and so when you're talking about basic things like how to avoid constipation and hemorrhoids and why am I bleeding, and those types of things you're trying to explain on an elementary level what you can do at home without spending the money and without the insurance and without surgery to help your situation. Even basic nutrition needs, eat more fiber, I say that every single day because they're eating fast food and they don't know. There's a lot of lack of education in our state that affects every single specialty.
[Dr. Oluyemisi Solomon]>> Agree with that because I work in Rocky Mount which is rural on paper. When you actually visit Rocky Mount it doesn't seem that way. But with my patient population it really does. My patients had all the same things you have no hot water, no water in the actual world. They don’t have city water, Well water, they’re doing that and they struggle a lot. But I would say the biggest thing for me with all everything else, I'm going to say its transportation. With me being in Rocky Mount like right in the middle between Martinsville and Roanoke and my patients don't want to go either way, they just want everything done there in Rocky Mount which is really hard. We don't have dermatology there, we do have general surgery there, which is pretty cool but we don't have dermatology, we don't have ENT. We had a Carilion pediatrics with doctor [inaudible] leading. But people that something's going on with that too. We don't have endocrine out there, [LAUGHTER] which is hard. So when my patients come in, I'm really that person to do everything for them, when they have a toe infection and they need that toenail to come off I can't send them to the foot doctor or the podiatrists because I don't want to travel. They may want to see the general surgery or the surgeons upstairs in my building, but they're also full and can't get them seen. They may need a Pap smear where they're having bleeding done, but they can't see GYN because there's no access, so I have to deal with that a lot. For those patients who have Medicare, it has to be done three days in advance to make their ride appointments and pick them up. If there happens to be inclement weather or I have to be out of the office for some reason and there goes their appointment and they can't get seen for the three or six months. And then of course they come with that long list again, so that cycle just repeats itself over and over again where they’re like, well, I can't come. And I have a fair amount of patients who walk anywhere from 5-15 minutes to come see me. And I really struggle with those patients now over the pandemic, I think we still are in a pandemic. [LAUGHTER] Over the past year, at least Carilion was authorizing the virtual visits, which was helpful for them. But now with the reimbursement being low, they're telling us to not do that anymore. So I'm having to say, I'm sorry, six months ago I could do everything for you over the phone but now you're really have to start coming in, and I struggled with.
[Dr. Olivia Asamoa]>> It'd be a lot of echoing what everyone else has said but yes, transportation is a big thing. Again, just having places where people can go like I had a lot of patients who need physical therapy for whatever reason because they live so far out, Roanoke is the closest thing for them and how are they going to bring a three-year-old to get PT when they have a five-month-old at home and there's only one car and dad has to go to work. So it's a lot of trying to figure out the best way to get people seen. But I think another thing for me is yes, there’s the education point, but there's a lot of misinformation out there too, just a lot of parents coming in, well I saw this on TikTok and this is why I don't want to give my kid vitamin K. I have to take a step back and fix my face because my face those things [OVERLAPPING] sometimes that it shouldn't But the mask isn't covering my eyes unfortunately. So it's just a lot of trying to educate your patients, I guess while the Internet is an amazing thing. It's a lot of great thing and there's a lot of misinformation on there and that's important when you're raising your own child. So I think that is a huge barrier a lot of times because lot of times they just don't want to do what you say because TikTok said, I should do this. Which sounds really silly when you say it out loud but [LAUGHTER] it is a barrier when you're seeing patients.
[Dr. Anthony Baffoe-Bonnie]>> I second everything that's said, I see that in practice quite a bit. One other thing I see as being detrimental to the patient's health and all confines is mental health. And we see the depression, bipolar and untreated mental health, and really, not letting patients avail themselves to treatments that would be simply effective for them.
>> [inaudible]
[Dr. Kemi Bankole]>> We have one more person who was working, busy and was late. Dr. Quarles, please come and introduce yourself and tell us about yourself and then answer that question as well.
[Dr. Calandra Quarles]>> So absolutely. My name is Dr. Calandra Quarles, I'm a hospitalist at Roanoke Memorial hospital. Hospitalist is usually internal medicine doctor or family medicine doctor who only practices in the hospital, and we don't see clinic patients. I'm not a primary care doctor so we don't follow over time. We see patients as they are admitted to the hospital, usually from the emergency room. So I can piggyback off of what some of you guys are saying because some of my issues are, what is the role of a hospital in their care? And so a lot of times they're here for an acute reason and they'll say, well, I've got a PT or I've got a CT scan that my PCP ordered or my OB-GYN wants to order this lab, can we do this while we're here? Though my heart is big and I want to do that, I would love it if we were a one-stop shop where you can get all the tests and all the scans that they can follow up over time. But that definitely puts it into perspective why, if you’rein Rocky Mount. But not if you’re in Roanoke for the thing that got you admitted to the hospital, and we tried to really focus and narrow in on that. So sometimes that can be just understanding the place of an emergency room and a hospital in their overall care.
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[23:24]: If you had a blank check, what would you focus on?
[Dr. Kemi Bankole]>> Thank you. So the themes I'm hearing are access , time, resources and also the support system on both sides, so for clinicians and for the community. So I've heard this question so many times, so if you had a blank check and you could do something about this on either side, what would you focus on? What would you zero in on?
[Dr. Sharon Williams]>> I really care about screening because for African-American people, particularly we tend to get certain kinds of cancers earlier while younger. You know what I mean, like the best example to me is colon cancer because I do colon screening. And I have come across a few people who are like 35, 45 and they come in at perforated colon cancer. I met one guy, I operated on him that night he didn't know he had the colon cancer. I came out to tell his family, his family went crazy because they had just lost his brother that week from colon cancer. And so if they had screened. If all the siblings had screened, that wouldn't have happened. So if I had money that I could just do [LAUGHTER] whatever I wanted with, I would make sure it's better education about the availability of screening would include like mammograms, prostate and colon, and then make the screening more available. And sometimes it's like you guys are saying is access like maybe they need wives. >> Yes. >> Getting a colonoscopy is a big deal because you got to be able to get all prepped, it's almost got it right.
[Dr. Kemi Bankole] >> And you have to have someone to take you there. You can't just go by yourself.
[Dr. Sharon Williams]>> Not just the money to get it done, but the access that you would need all that. Someone needs to stay with you afterwards. I would work on screening, prevention type of things.
[Dr. Kemi Bankole]>> Thank you.
[Dr. Ayesha Kelly]>> I would love to see more of you, more doctors, more nurses, more psychiatry. All these specialists that we are missing, all these family practice folks that we are missing. I feel like we are behind the ball in getting enough people trained to see the amount of people that we have. We have a nursing shortage in our hospital, I'm sure that all of you do. And a lot of times there's enough money for nurses to pick their best, the highest paid, or to travel, there's a lot of people traveling because there's not enough to go around. So we're struggling with just having personnel in every level; radiology, environmental services, everything. If we had more money to pay people better and to train people, we would fill the gaps that are so profound in every single section.
[Dr. Kemi Bankole]>> Thank you.
[Dr. Anthony Baffoe-Bonnie]>> So the question was if we had one wish?
[Dr. Kemi Bankole]>> No, you had a blank check.
[Dr. Anthony Baffoe-Bonnie]>> Blank check.
[Dr. Kemi Bankole]>> What area would you focus on either on the clinician side or on the patient side that you would help fix basically?
[Dr. Anthony Baffoe-Bonnie]>> For me probably is meaningful education and information to patients. Because when you give them that then they are able to find resources which they would otherwise not have. They would be able to know what type of test they need to do. So that meaningful education is important, health education for our population generally.
[Dr. Kemi Bankole] >> Who wants to go next?
[Dr. Oluyemisi Solomon]>> I'm all about screenings [inaudible], that is something that I think I do regardless [inaudible] like nobody walks out of my clinic without knowing if their test came [inaudible] chronic smoker. [inaudible] I find that a lot of my physicians colleagues not in pediatrics [inaudible] a lot of people probably shouldn't. If I smoke [inaudible]. We still have to follow up with them and say, hey, if you’ve been smoking for these many years it leads to lung cancer. But also that they want something done about this, But what they don't want is to do is screen and [inaudible] [OVERLAPPING]
[Dr. Kemi Bankole]>> And then not do anything about it. >> And not do anything about it [inaudible]
[Dr. Calandra Quarles]>> So in this scenario, I have two blank checks. >> Go ahead. Yes. >> So honestly education but in a different twist. I would say medical education. So if I could build more medical schools, train more physicians. I think right now we're in the surges of physician extenders and nurse practitioners and PAs, which I love them. They have a role but I wish I could put more money towards medical education, more medical students, more residency spots, particularly on that first blank check.
And then the second blank check would be prescription coverage. We miss that sometimes. It's like we diagnosed the treatment, we got it. Here we go, let's go. And then either they don't have insurance or insurance doesn't cover it, or it's so super expensive, who could cover it? Even with insurance, hundreds of dollars a month for something you need. And then we have to be like, what's the secondary? What's the second line of treatment? What's something we can get around it. I wish that was a non-issue, like they just afford what it is that we say they need and that's all within whatever is reasonable price point difference.
[Dr. Kemi Bankole]>> Thank you. That's a really good one.
[Dr. Kimberly Clay]>>So if I had a blank check, what I would do is pretend I was Oprah. I would make multiple medical clinics where they actually have every specialty that you need that you'd have mental health, primary care, OB, surgery, and you have a pharmacy where all the medicines are free. And then you'd have mental health, endocrine, I mean, everyone, cardiology. And you would get to see any specialist that you need. So somebody would come in primary care, do an intake. And you'd be here, just like you have in Cleveland Clinic, you'd stay for a couple of days. We got to somewhere to stay. There's a hotel. We got you some TV and some cable. She knows how much the cables important [LAUGHTER] So we'd make sure this would be a two or three-day thing. You'd get to see everybody, makes sure you had all your follow-ups, all your scans, you'd have your medications, everything would be taken care of. And these clinics would be everywhere. So it's not like you have to go to Cleveland to find it. So based on the population of the city, we'd have many clinics that we need for that population. That means anywhere from Martinsville to San Diego, we'd just everyone have one so we'd have access. So if I had a blank check, health care would be free and we'd have all all these things taken care of that will all be addressed at one time. >> Same thing.
[Dr. Olivia Asamoa]>> So to go off of that. I think that would be awesome. I think more education in schools. It's just about just general health. There are a lot of kids who come in and I feel like maybe it's just our patient population, but obesity is a huge thing in our patient population. And it's just like, oh, well, it's just what we do. I think obviously we don't have enough time, but if time wasn't a thing, I think just more general education in schools about what living a healthy lifestyle looks like and that could be anything from like food education, that could be mental health education, because a lot of kids, when we talk about, hey, do you have a therapist or a counselor school? Oh, well, yeah but I just never thought to go talk to them. Like, well, do you like this person? I'm good. I think they're fine. But it's like they don't take the time to go and talk to them, thinking that this will be helpful for them. A lot of kids are going through a lot of things at home they can't talk to people at home about. I think just having more education in schools, just more resources for kids at school because it's like they're already there for 8 hours every day. So why not take the time to actually help grow these people into healthy functioning adults.
[Dr. Brooke Watkins]>> So I would, because it's my passion, make a lot of different changes for maternal health in general. So making access to care, transportation, daycare at the visit, maybe, something that makes it easier for them, doulas for everybody [LAUGHTER] Honestly, I'll probably make labor and delivery like a spa like experience just so you can come in and be relaxed, play some nice music, do all the things, but just make it better for moms because I feel like the moms are super women and their access to care and just care in general, maternal mental health, I would focus on that. There's a lot of things. I'll do a lot focused on just women. I'm actually sorry, man [LAUGHTER]
[Dr. Kemi Bankole]>> I think I'd like to chip in here. I have this small thing that I think I would want to do, and that is increase community participation in health. So starting with our kindergartners and moving on to get our students and children in our own community to be interested in becoming physicians and physical therapists, occupational therapists, nurses. Because when we have folks like that in the community, they're more likely to stay in the community and help the community. We already have two residents, two physicians here on this panel, this August panel who complete a residency here and are contributing to the community in that way. So I want to build that up so that, because they're from the community, they will know what the needs are, where the pressure points are. For me, I think that is just one thing that I would spend my blank check on.
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[33:56] What are myths about your specialty that you would like to dispel?
[Dr. Kemi Bankole]>> What are myths about your specialty that you would like to dispel. Something that someone says and you hear it over and over again and you don't know where that is coming from. Or maybe you do know and you're like [OVERLAPPING] Yes.
[Dr. Kimberly Clay] >> [inaudible] [LAUGHTER] [inaudible]. You’re going to judge me based on how I eat. [inauble] I’m trying to figure out how can we make your health better, the dietary choices. Not only are you [inaudible]. Second, [inaudible] The reason why I say that is because so many people come to me about thyroids and two colon cancer, one gallbladder cancer, two ovarian cancer. So many… and I feel like that’s part [inaudible] and that’s my two points of how people go home and they talk to [inaudible] and then you find out there was something else they want to delay [inaudible] details about thyroid, I’m ordering a CT scan and find pancreatic cancer [inaudible]
[Dr. Brooke Watkins]>> Oh, Sorry. I have a few as well, not as [inaudible] answers, but I think the first one is that you don't need to see an OB-GYN unless you are childbearing. Because we get a lot of people that come to the OB-GYN, they have their babies and then we never see them again. And there's a lot of things that happen, menopause or post-childbearing, that people are not educated about like urinary incontinence, that's not normal. You can do something about that, but people just leak urine and they're like, Oh, it's fine, this happens after babies. And then, also on the opposite side, you can come to see us before you’re 21 to talk about contraception, safe sex practices. That's also a thing. And there was another one that I can't remember, let's see. I think those are the big two. Also, that birth control affects your fertility that's not true as well. I get that all the time that they don't want to go on birth control because it affects their fertility. I think that's it. If I think of the other one, I'll say.
[Dr. Anthony Baffoe-Bonnie]>> One myth I would like to clear is antibiotics don't do nothing for your viral respiratory condition. And it's not unusual to seek care and say doc my sinus and into going to my chest and that's when I get pneumonia to try and get antibiotics, but we know that it doesn't work and it actually has bad deleterious effects. So that's one myth I'd love to clear.
[Dr. Ayesha Kelly]>> I would love to dispel the myth that if you're seeing a surgeon, you're getting cut on because not everything needs a surgery. And just because you're seeing a surgeon doesn't mean you need that particular surgery. And I have lots of patients who come in very anxious because their PCP or whoever else has sent them to a surgeon and they immediately assume one that they're having surgery or two, that they're having surgery that day or they're coming in and we're coming to talk about a colonoscopy. They are mad that they're not getting their colonoscopy that day. But you had your ham and cheese biscuit that morning. You're not getting a colonoscopy today. So that's it. Or you have gallstones and they found it while they were looking at your IUD in your uterus and they found you had gallstones and now I'm coming to have my gallbladder out because I have a stone but I've never had pain there. You're not coming to the surgeon to always have surgery?
[Dr. Sharon Williams]>> The surgical thing. I think it may still be true, but for a long time, I was the only female surgeon that did hemorrhoids in Roanoke. So I was seeing all the people with bottom problems. If you have blood in your stool is not necessarily hemorrhoids. So I want everyone to know that. You need to get checked, be assured that it's not going to be cancer or a tumor, but they're actually a lot of other things I can't tell you how many people have argued with over the fact that they don't have hemorrhoids. [LAUGHTER] I had that argument yesterday, literally yesterday. But the one thing I would want anyone in the community to know. If you have blood in your stool blood when you wipe go see a doctor. It doesn't mean you have cancer. It doesn't mean you need to be scared, but you do need to be checked. So go and see someone and get checked so that you know. So that's the other myth. It's not always hemorrhoids.
[Dr. Olivia Asamoa]>> I think one of the biggest ones are that kids are little adults. That is just so frustrating because it is not true. Then it's, well, I have this problem and it's about them. And it's, no, sorry, there's a reason why I didn't do adults. Please don't ask me. You don't want me, no sorry. Or parents who are giving their children adult dosing and medicine because they're little adults. No, there's a reason why there's different medicines for children, a whole thing. I think my second one is just for my OB colleagues, is that new moms will come in and tell me all the things. If not about lactation, I can't help them. And so a lot of times I'm just encouraging like, "Hey, have you called your OB?" No. "Could you do that?" It's because a lot of times they don't have a PCP and the OB is the last physician that they've seen. So sometimes I wonder, I'm like do I need to take a crash course in OB like post-birth because I have a lot of moms asking me a lot of questions that I just don't know how to answer?
[Dr. Brooke Watkins]>> That’s another thing. After you have a baby, you need to come see me. And a lot of people don’t.
[Dr. Oluyemisi Solomon]>> [inaudible] [LAUGHTER]
[Dr. Ayesha Kelly]>> This happened to me before residency. I did a residency here too. That I lost my insurance as my child got insurance, as my husband's insurance would cover one of us and not both of us. And so sometimes the mother may be not insured and that's the only opportunity you have to ask questions. Now, obviously, I did not do that because I was uneducated. [LAUGHTER] But I think that's part of the problem is once you lose your insurance and that child has the insurance fee. That's the only physician, you're going to see. >> That's good to know.
[Dr. Oluyemisi Solomon]>> An interesting one I get, well, let's do it this way from the general population. We hear this a lot, that family doctors are not real doctors or they're not as good as specialists. So we don't have to go see a family doctor if we could just see a specialist. That is not true. We are the gatekeepers of medicine. We are that entry point. Forget the fact that most insurances want you to have a referral, to see a specialist. Not that urgent cares are not doing the ERs are starting to do some of that, putting in a referral, and that I really do appreciate it because it jumpstarts that process. But no, we are real doctors. We're not GPs, GPs are general practitioners. They did go to medical school but they did not go through residency. There's a big difference, they're not certified by the medical board. Family medicine is. So we're not one and the same. Your PCP is not AGPOSARHP, PCPs, I think GYN sometimes falls under that category of PCP. So there's that. And the other thing for my actual patients, don't just come see me when you have a cold and you want antibiotics. [LAUGHTER] It's always this thing I woke up with a sore throat this morning, please let me [inaudible] It's only been one day. I understand your concerns. Can you give me a pocket prescription? No, we don't do that anymore. But you did during COVID? I know, because we weren't seeing patients in the office. So please come see me regularly for your routine things. And just because you have a sore throat or a cough or a sinus infection, which can be viral to in the first week. You don't need antibiotics but come in for regular health maintenance for screenings and for vaccines.
[Dr. Olivia Asamoa] >> [inaudible]
[Dr. Kemi Bankole] >> Well, I will say this. Anyone that says any part of medicine is easy as just wrong. There are so many complexities and I really grateful for the fact that we have different specialties for people to specialize in. Because you wouldn't want me as your OB [LAUGHTER] You wouldn't. For me in psychiatry, one of the myths I would like to dispel is and as a geriatric psychiatrist, I get a lot of older folks and they have more of societal thoughts and misgivings that's been baked in for decades. And that any mental health is a moral failing. It is not. Specifically in older adults, being depressed because you're 75 or 85, that that's normal. That is not normal. Being depressed at whatever age is not normal. Because you will have folks that they'll just be depressed and they're just live with that. And Dr. Baffoe-Bonnie talked about how that affects so many other things with regards to health care. And we know that with depression specifically, that you tend to have worse outcomes if that's left untreated regardless of what it is that they're treating. You have a heart attack, if your depression is untreated, you have a worse outcome. What does your heart attack have to do with depression? But studies have shown that you have a worse outcome. So for me, mental health is not a moral failing, it is an illness that is treatable. And that those treatments can vary. So it's not just medications. Sometimes for me, the treatment I prescribe for my patients is physical activities, exercise. That can be what someone needs. Treatment and management is varied, it's not just medication. And we know the psychiatrists, we try and see as many folks as we want. And we'd love to have more medical students go into psychiatry to fill that shortage.
[Dr. Brooke Watkins]>>I'll add something I just thought about not all vaginal discharges are defects [LAUGHTER] If that was not clear. If you're having anything, and it doesn't go away just let us know or ask to come see us we have a lot of things that we can do for you.
[Dr. Calandra Quarles]>> I'll add to my specialty. So you'd be surprised how many people think we say hospice. When we say hi, I'm a hospitalist taking care of you today and they hear hospice, and they're like, what's happening? [OVERLAPPING] I will have to correct once a week. It's surprising how often that happens. So then I go no, internal medicine or family medicine in a hospital are given the title hospitalist, so that's an odd. Then the misconception that I'm still sick, why are you sending me home? And that comes up a lot. We're like you're sick, but stable the need for hospitalization. I'll say that a lot like you don't need IV and pain medicines and monitors anymore, you're stable. I'm not saying you're not sick, but we're going to let your primary care or your next clinic-based doctor come in and from this point, but why are you sending me home? I'm still sick, is almost a battle. And then the opposite is Well, you didn't do anything. I get that a lot. Well, we did. All this million-dollar workup. Thank goodness it’s negative, and I'm glad we found nothing so then you can have to leave the hospital like that.
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
[Dr. Kemi Bankole]>> All right. Thank you. So what changes? And we've talked about a lot of things that need to change. That we would like to improve with a health care system.
But from the time where you were training as medical students, during residency, during fellowship, what changes or improvements have you seen, observed in your field during that time?
[Dr. Ayesha Kelly]>> I've been waiting for this question [LAUGHTER] And I can't say that it's improvements, but I am going into my ninth year of practice. And the first five years of practice, everyone says are the worst in terms of learning, and growing, and knowing what you're doing and feeling comfortable. My first five years were like that, but then COVID hit. And so my most recent three years have been in a rural setting with COVID. COVID has turned us upside down in our facility. It was the single most horrifying part of my career thus far. To give an example, we had regular bread, butter, I'm doing scopes, I'm doing hernias, all this stuff, I went to West Virginia for vacation in March and I came back to, all my cases were canceled and I'm helping my partner with a colon cancer. That's the only case that's happening in the hospital and we had an empty hospital. We had everyone there with nothing to do for the first few months because we did not have the surge. And we had people being laid off or furloughed waiting for the surge that was supposed to be coming. And we were seeing people from home and as a surgeon seeing someone and asking them to describe something, when we have a rural community with no video capabilities, either in the office or at home and patients who don't have smartphones and it was a crazy thing. I got lots of time with family, but it was awful. And then when the surge finally did hit, we had patients who had no business being in our 25 bed critical access hospital that we couldn't get anywhere. I mean COVID patients with duodenal perf, who I'm taking to the OR because nobody else will take them, no one has ICU beds and they're lingering can't get them off the vent because we have no surgical intensivists and we have no prayer of providing the things that are needed, or having to tell a patient that you need dialysis, but we can't get you anywhere because there's nowhere. Being on the phone talking to other surgeons who wish could help you, but we don't have any beds. And so our acuity went through the roof. We were losing people who maybe have a death or two every three months. And now we're seeing people die every week. And so it's hard on the staff and everybody knows everyone. And so that perforated ulcer is my environmental services mom. And that perforated colon who's had colon cancer or who's had COVID for weeks, and has liver failure and we can't take him to the ICU or can't take them to the OR he's just too unstable. I'm singing of him because they know me and they want me to sing their last hymn on face time. Those types of experiences I will never forget. And it has forever changed medicine for me. It's better, but you're still waiting for the next surge because you know that our community is full of elderly people. We have lots of nursing homes and you know all these people, and they are your friends and family and moms of friends and it's like losing people that you are close to constantly, or feeling helpless because you can't get people where they need to be. And that has changed everything for me. I'm still like, we're great now, we're moving but there are days where we don't have beds, and you still have to look at your list and say, are we going to be able to do this surgery today because we don't have beds to put this person in and should I be doing nine scopes today when if anything happens to any of them, we don't have a bed to put them in? So it changes the way you think about everything that you do.
[Dr. Kemi Bankole]>> Thank you [OVERLAPPING]. >> I'm here.
[Dr. Kimberly Clay]>> We can bring it up just like most people, sugar. [LAUGHTER] I think, I've been practicing 14 years now, so it's been a long time. So when I first came, we didn't have continuous glucose monitoring, you had to do finger sticks and that's pretty much what you had. I'm not saying I was on the cusp of just having NPH, but I'm going to say I'm pretty close. Lances actually had just come out probably about two or three years, actually by the time I was a resident. So having long acting insulins, even better fast acting insulins has made a world of difference for our diabetic patients. Pumps, before they were like book bags. Now, there are actually small things that are smaller than your phone that you can attach. So there's been a lot of technology, especially in the diabetes world, that's really been great. As far as procedures in my first thyroid biopsy, it was blind, I wasn't blind folded, but [LAUGHTER] it pretty much could have been the same thing because we had no thyroid ultrasounds back then, you did it all at the bedside, and it was palpation and go, and let's just say my first one didn't go so well. [LAUGHTER] Patient is fine, just make sure everyone knows, patient's fine, but there was no adequate specimen there. So luckily now we have ultrasound, we have ultrasound in clinic, I can do that actually in my clinic, which is fantastic. So that's an advancement, so the upside, obviously, of things. So hopefully that not only sugars, but ways to control sugars have improved and gone up as well.
[Dr. Sharon Williams]>> For me in general surgery, we've gotten a lot better with our laparoscopic capabilities, and we've added robotic surgery. For me personally, I didn't think robotic surgery made sense because I was a really good laparoscopist, so I was like, why do I need that? Then I started to do some of the surgeries and the ergonomics for me is amazing, because laparoscopic surgery you have to contort yourself and do all these weird things to get things done to these tiny holes. Robotic surgery is still laparoscopy, which I need to clarify because suddenly we're like, well, you will let the robot do my surgery? No, I'm going to do your surgery, I control the robot, that is my robot. So it allows me to have a little wrist inside of the patient, and that saved my risks. So that has been amazing. We have much better mesh. So you remember hearing those commercial, did you have a mesh hernia repair? Did your life end? But you're still here watching a commercial. There are a lot of the measures that we used to have weren't good, and we didn't know that because we just started putting them in and we did the studies, and now we've learned a lot about mesh, we were coating the mesh, not having it be two pieces, no solid parts, dinner meshes, meshes that are more resistant to infection. They just recently got us the suture that is antibiotic, so we have that here now. There's a lot of things happening all the time, just amazing things in surgery. So I'm excited because I feel I'm right in the middle of my career where I can still see a lot of more things, because I've been at it 13 years. So I got another 15, 20 to keep doing stuff and see what else happens.
[Dr. Olivia Asamoa]>> I guess I can go real fast. So as someone who's been doing this all of five-and-a-half months. [LAUGHTER] Let's see. [LAUGHTER] I think the biggest thing that I think was a plus with the pandemic was we're getting access to mental health services because everything went virtual. So I think that's been a huge game changer because again, a lot of patients are living in further places and just don't have access to clinical psychologists, so I think that's been a huge game changer as that patients are able to see therapists and psychologists from home granted if they have internet connection, which is a whole another thing altogether, but I think that's been a huge positive from the pandemic, if I'm allowed to say that little.
[Dr. Oluyemisi Solomon]>> And I'm right on with that too, because the big thing I was going to say is eConsults. Again, for me, family practice, a lot of it is knowing my limitations and what are okay, I've done this and this for you. You have to see a specialist. They don't want to, but I'm telling them they have to, but they still can't get there. So eConsults have been a big game changer in this past year from whether it's infectious disease or a pharmacy consult for cost of medicines because sometimes GoodRX just doesn't cut it. I'm spending 10 minutes plugging in every medicine to GoodRX with my patient in the room in a 15-minute appointment. [LAUGHTER] So that's been helpful. Dermatology, oh my goodness, that is so good. I can take pictures with my phone, put in Epic, send to the specialists, they get back to me, tell them to take this cream, if it's not better, they can come see us. Oh my God, that is life changing, it's great. So eConsults, it's been the biggest thing for me.
[Dr. Brooke Watkins]>> I also have not been practicing that long, so good year needs some change. So not as a lot has changed in OB-GYN since I've gotten out of residency. I can say the IUD, which is a great form of contraception, is now approved for eight years, the Mirena specifically, so if you have one, keep it in. [LAUGHTER] But I think the biggest thing, which is not necessarily, I think we're trying to change it, but the biggest thing for me is the emphasis now that we have on Black maternal mental health and mortality. It's become a huge topic right now, and I think we're paying a lot more attention to it, which is great because it's been an issue since gynecology was founded basically. So I think with now the turn of us trying to have big initiatives like ACOG, the big societies in OB-GYN in general are trying to do better, and I think as more people become aware of the issue that more people are actively trying to do better, and I see even my non-minority colleagues attempting to actually pay more attention, be more intentional about how they treat pain or listen to patients, request their needs and concerns. And so I think that's the biggest thing that I appreciate that it's changing with an OB-GYN around, because it's a huge issue.
[Dr. Anthony Baffoe Bonnie]>> I'll add interdisciplinary is that ok. I've seen that become more paramount of work. Prior to pandemic or a few years ago, you would have one provider do everything, but doing let's say, with hospital acquired infections, it could be just their nurses taking care of business. The provider is so called oblivious for it. I see in medical schools there's now discussions about how interdisciplinary teams work, and even on the units I've seen a lot of good communication between teams because at the end of the day that really is what benefits their patients. So that's one bright spot. And I saw quite a lot of it with the pandemic, there's a lot of things that different teams from IT to finance, to EBS staff are working together. Interdisciplinary version really helped.
[Dr. Calandra Quarles]>> I can echo that. I am in my fifth year now. And, so not too much in history. The medicine is the same as it was, but just the team approach is the standard. You're not going to be a cowboy, you're not going to be the one guy doing everything, and so everybody's voice is as important. Social worker, I need to hear from her, PT, I need to see what they're saying. And so it's kind of that whole team approach is the standard, the doctor is not running the show. That's like a misconception. You can have all team players contributing different roles. And then also the technology, I think COVID forced us to be a little more to tele everything, and then we'll hear tele hospitalists, they'll tele PCP appointments, and so that's new, and I hope we don't get too carried away. [BACKGROUND] [OVERLAPPING] tele ophthalmology appointments. I had one myself and I was like, this got weird. [inaudible] so yea, technology, and team based.
[Dr. Kemi Bankole] >> Thank you all for all of that. And I'd like to echo some of the things that folks have said. I've been at Carilion almost 14 years, and I remember when I first started straight out of fellowship, the Department of Psychiatry had a project, a research project, where we're figuring out whether doing telepsychiatry in the emergency room was as good, would give you as good outcomes as seeing evaluating that patient in person. And we found that that it was, I mean, within a couple of years, and all of the psychiatry attendings were involved, and you could be called at any point in time, and then you'd ask, am I in the ER or am I in the room with the video, with the TV? So even back then we knew that this was a good way of evaluating patients. And it wasn't until the pandemic where that really just supercharged that. So that's for medicine as a whole, but in psychiatry, one of the things I will say that I have seen change is people's attitudes to mental illness. And people are more open about talking about it. There's still some things that are lingering, but talking about going for therapy, it's less and less being frowned upon, and I think that's only a good thing. So I want to give a big thank you to our panelists for answering my questions. [LAUGHTER]
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[1:05:11] What do you wish you had learned in medical school or during residency?
[Dr. Kemi Bankole] >> And I'm going to leave questions out to the audience, if we have any questions either in person, or who's taking care of the chat? Questions from our audience?
[Audience member Elvir Berbic] >> Hi, everybody. Thank you for being here. And I appreciate you taking all the time to come here. My name is Elvir Berbic. I work in Student Affairs here at the medical school. So our goal is just making sure that students stay above the water. But at the same time making sure that they're heard, they're understood, and they're being a part of their experience. I want to ask you something that you hinted at on a couple of times about education, but about your education this time. So what do you think in terms of changes and what things we can implement in education, specifically in medical education that you would think help this community? That you would maybe would have seen in your own experience. So I just leave that out.
[Dr. Sharon Williams]>> [inaudible].
[Dr. Ayesha Kelly]>> For my education, I would have, not necessarily medical school, but it would have been helpful too, but especially for residency, better mentorship program, especially for as an African-American female. We had several African American female residents. We did not have any attendings, Dr. Williams you weren't here yet. [LAUGHTER] Sorry to have missed you. But there were very few females and there were no African-American females and our African-American males were at New River Valley. And so it was tough being the only or not having someone that could provide mentorship in a way that addressed all of the issues that you're going through at the same time. So I think that we even virtually if we were to do a better job of matching minorities with a mentor even if you don't have those mentors acknowledging that you need those mentors and finding a way to bring mentorship to your program would be great.
[Dr. Kimberly Clay]>> [inaudible]
[Dr. Kemi Bankole] >> Can you make sure that the mics are on so that the folks on Zoom can hear. >> That was also helpful. [LAUGHTER] >> Can you pass the mic?
[Dr. Oluyemisi Solomon] >> When we talk about finances, you need to learn how to manage your own finances. But this is not for general population but for the students. Yeah, that was your question. Coming out and the income you make in residency is completely different from what you make before. But for those of us who did not have professional careers. Then it's one thing being thrown into the real world. You're like, whoa, that doubled or tripled on me. And it's time to file taxes and we have no idea what we're doing. We don't know how to write off our expenses, how to cut things down. A lot of us have student loan repayment things. A lot of us have spouses who are also physicians, and then we struggle. Should we do this jointly? That was a bad idea this year because now our loan repayment goes way up. Or should we do it individually or things like that? I think that would have been helpful for me in medical school and residency to know that this is how you should do this. Try not to take all the student loans if you don't need it. Because once [inaudible] I finished out of residency that's six months and they’re like, oh, we want our money back. You're like, how? And it's really hard. And everyone looks at you're a doctor you make so much money now. It's hard. No filter here, but I have 50 million kids. I want three. And I would share this, childcare with Honey Tree last year was expensive. We spent over $25,000 in childcare. Yes, that's a lot. That for some people that's almost their annual [income]. And then it makes you wonder why people stay home and don't work. My husband is a physician. I look at him and I say, oh, here's where all our money is going so who's supposed to stay home. And he looks at me like maybe you. [inaudible] It's too early, I'm not doing that. So here we are, so no more kids is that, that unless the moral here. [LAUGHTER] But we also don't have any family in the area at all. It's just me and him and daycare, but just thinking about that and knowing how to manage our finances, knowing what to expect after residency, after academic training.
[Dr. Sharon Williams]>> To piggyback on that. I don't know if you guys have this, but when I finished my residency, one of the most helpful lectures I had was one about contracts, like signing contracts when you leave residency to make sure they don't gyp you because they will because I know you don't know any better. So Dr. Clay was saying things about billing and everything, but telling them what they should expect to be paid and how to negotiate that is super-helpful. So I don't know if that's something you have available.
[Dr. Olivia Asamoa]>> Access for them or if there's any resource or websites are like, hey, this is what you should look for in a lawyer who's going to review your contract going forward. I think that would have been helpful too.
[Dr. Ayesha Kelly] >> And to add to that how to find a job. Because once you've finished residency, you have to find a job. And I did my senior lecture at the end of residency on how I found my job, which was completely unconventional. Going to hospitals and saying, hey, y’all need a surgeon? Yeah, literally that's how I found my job. But no one had ever talked to us about how to actually finish residency and start working in the real-world. If you were not going to work in the place where you did your residency, where are you going and how do you figure that out? It would be nice to know before your last year of residency.
[Dr. Calandra Quarles]>> And a little different. So one of the benefits I think I got for my residency there, I don't know that everybody does, is we had disability insurance lecture thing and the guy actually came and signed us all up for disability insurance and before we graduated. So we've got this super low rate that doesn't ever change and you're more young and in good health. And so we've got disability. What do you call it? It all out perfect set up as a resident. I don't know that everybody is residency was doing that, but that was a nice little touch.
- [1:32] Introductions
- [4:02]: What are some of the challenges you face in your day-to-day practice?
- [14:07] What about challenges that you have seen or noticed that your patients are facing on the other side that's acting as barriers to ensuring their overall health?
- [23:24]: If you had a blank check, what would you focus on?
- [33:56] What are myths about your specialty that you would like to dispel?
- [48:45] What changes or improvements have you seen, observed in your field since you were in medical school, residency, or fellowship?
- [1:05:11] What do you wish you had learned in medical school or during residency?
- [1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[1:15:16] How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[Dr. Kemi Bankole]>> Thank you. All right, so we have one question here from our virtual community. How can white members of the community help support efforts to recruit and retain black physicians and healthcare providers?
[Dr. Anthony Baffoe-Bonnie]>> I'll start off. Being an ally is always an important thing and being a meaningful ally is. So in communities where you couldn't go to high schools, pipeline for how kids even get into college and then to medical school to begin with. Where you are able to talk to other children or high schoolers about medical school, your experiences. And that's helpful. So I think that's one area of the pipeline that working in is going to be helpful for us. >> Thank you.
[Dr. Kimberly Clay]>> So another thought, I would have to agree with everything you said. I think having a supportive environment and that is very important, for someone who has worked a couple other places in my 14 years. One, I would say definitely about Carilion. This is the most supportive place I've ever worked. Where, no matter what ethnicity my colleagues have, I feel like I'm heard and supported. I haven't always had that. Sometimes you walk in the room and as we all know, you already get judged before you even open your mouth and introduce your name. And so having people understand that and understanding our perspectives can be very important. I think interacting with each other, interacting with patients, staff, employees. And I actually Sharon and I both did a talk about diversity, where we talked about not only from a medical studentstandpoint, but from my personal stories, her personal stories, things of that nature. And the thing I got from my chief was, what can we do to help you? What can we do to make this a more supportive environment if things were to occur? And the fact that someone took that perspective to me is one of the big steps that you want to have. To understand that we all are different, no matter where you come from, what your background is. And take the time to get to know everyone and not just look at how they look on the outside, but learn them on the inside as I like to say, I think that's really important. We have colleagues that do that. I think is really good.
[Dr. Sharon Williams]>> One other thing which something Dr. Kelly made me think of is that, if you are a white physician and you have young black people who are into your purview working with you, you can be a mentor too. And this is really important because of the limits that are enforced on minorities, we would not necessarily have the connections that you would have. So as somebody's mentor, I do have a more limited range. That's life. But as opposed to if you are a chair of your department, or if you are just a senior member of that department, you know everybody there. People can have more than one mentor. So if you see a young black female resident in your group, just reach out to her and introduce her to people that you know, or people who you think can help further her education, or people that might be able to help her understand something that she maybe needs to know or whatever, or maybe who works in the area that she wants to work. So I think mentorship is not just limited to us for us. Actually, for it to be better, our allies would be mentors with us as well. So that's one thing that it might not be that hard to do because you don't know they need you. So just reach out. They are not going to ask. Just reach out and say, hey, let's talk about how to get a job. And just sit down and talk to them about it like that. So that's the other one that I would mention. >> Thank you.
[Dr. Brooke Watkins]>> I think support is huge and mentorship as well. But on the opposite end, I would say, don't always assume that the minorities want to be the champion for the community. Because we do so much already and we have our everyday struggles as well. And so it happens a lot if you're the only minority or one or a few that you automatically assume that you're the champion for the black race. And so sometimes that can be trying for sure. So I would say just consider that as well. We need support. We need mentorship just like everybody else, but we also don't need other burdens on us as well.
[Dr. Calandra Quarles]>> I was going to say, because there are paid professional consulting services, they can come in and do the diversity training. You don't have to ask that one black [LAUGHTER] co-worker how to diversify my unit. There are organizations who do that and specialize in that. That might be a better way to do that.
[Dr. Kemi Bankole]>> I want to add to that, but if you are doing something that it is important that the work that you're doing is highlighted, it is rewarded, and that reward can be financial as well. I'm just saying. [LAUGHTER] [Dr. Ayesha Kelly]>> If you are an ally and you want to be involved, joining the diversity groups that are forming under whatever umbrella Carilion's doing it to joining black societies, we got the Society of Black Academic Surgeons, you don't have to be black to be a member. You can be an ally and be a member, and shoulder to shoulder with black surgeons, and see who needs help because they have students and residents coming in too. So you don't have to be a minority to be a part of a minority group. In Lexington, we have NAACP, it's half white, because we don't have very many black people. And it's great to see other people getting involved in organizations that are traditionally just for minorities.
[Dr. Kemi Bankole]>> Well, I want to give our panelists here a big thank you. Can we just give them a round of applause for all that they've done this evening? Great. Thank you. And for folks that are in the room and are online, we have compiled a list. It's not an exhaustive list. We'll be working on this and updating it, black physicians in the area, not just with Carilion, but with LewisGale and other providers. And if you have any suggestions or recommendations to add because there'll be a living list, so they will be updating that for folks. So that is that. We have paper copies in the room and there should be a QR code placed for folks that are with us virtually. Thank you all for helping make this event. I think it's a success. I'm really glad with all the information and what you've shared with us today. And hopefully, we'll see more people coming into medicine so we can deal with some of these shortages that we've been talking about today. Thank you, everyone.
Statement about accessibility and accommodation
The Virginia Tech Carilion School of Medicine is committed to creating an inclusive and accessible event. All virtual events will have automated captions. Recorded events will have edited captions available soon after the event. If you desire live captioning or a sign language interpreter, please contact the organizer two weeks before the event.
For in-person events, the main VTCSOM building at Riverside 2 is wheelchair accessible from the elevators inside the parking garage. Blind or visually impaired users may need assistance finding the elevators under the building, or using the stairs in front of the building.
If you need a reasonable accommodation to attend an in-person event, please contact the organizer of the event. All reasonable accommodation requests should be made no less than 2 weeks before the event. We will attempt to fulfill requests made after this date but cannot guarantee they will be met.