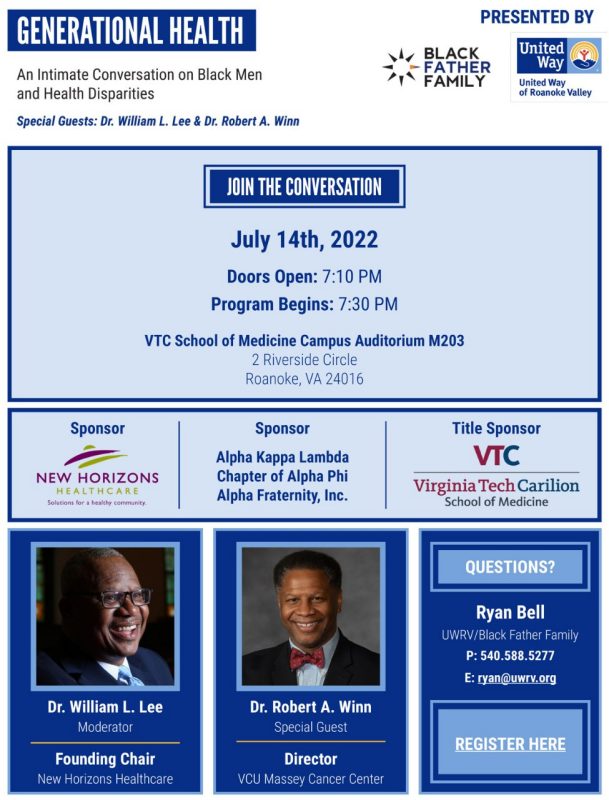
Generational Health: An Intimate Conversation on Black Men and Health Disparities
July 14, 2022

When
July 14, 2022, 7:30 p.m.
Where
Auditorium M203
Virginia Tech Carilion School of Medicine
2 Riverside Circle, Roanoke, VA 24016
Contact Info
Ryan Bell, Black Father Family at ryan@uwrv.org.
[Ryan Bell, founder, Black Father Family]: All of the work that we're doing at Black Father Family, we position it from the lens of public health, right? How do we, as black men, as black fathers, begin to prioritize our health? We can't leave a legacy if we're not here to leave the legacy, right? So I thought it was critical for us to begin to have that conversation.
[Dean Learman]: VTC is a perfect place for this event because it demonstrates the commitment that we have and to really establish trust that we are here to build solutions as allies in our journey toward a more equitable health system.
[Dr. Robert Winn, director of VCU Massey Cancer Center]: Science is great. Technology is great. But the reality is our job is to make sure that we don't lose the one most valued thing. And that is public trust. We have to make certain that we're communicating and that we're showing as health system or scientists that we care. And particularly when it comes to African American fathers, and this program really is centered on how to get men's health back to health. So these types of conversations are setting then in the motion of maintaining and even rebuilding and gaining public trust. And that's why participating in these types of conversations are going to be critical, not just now, but in the future.
Watch the full event
Video Transcript
This video transcript has been segmented into various pieces, beginning with introductions. The conversation between Drs. Lee and Winn are segmented by question, as are the questions posed by audience members.
[NL Bishop, Senior Associate Dean for Diversity Equity and Inclusion and Chief Diversity Officer for Carilion Clinic]
Good evening everyone. Good evening. I'm NL Bishop. I serve as Senior Associate Dean for Diversity Equity and Inclusion here at the Virginia Tech Carilion School of Medicine. It's good to see you-all here. I'm looking out and seeing people I know from so many different places; friends and colleagues who I've worked with and known for many years, and we're just delighted that you're here from so many communities, people who I've worked with and people from faith communities, fraternal organizations, and social services organizations. It's just great to see you-all.
I'm going to be calling up Dean Learman, who's going to come and give us a welcome. It has been a real pleasure for me to be serving in this role and working very closely with him at this fine School of Medicine. Dean Learman came here in 2019 and has quickly immersed himself inside this region, not only here but across this entire region. He's been doing some really great things inside this building, working with students and faculty here, producing medical students who are going to go out and serve wide and far. But not only that, the things that he's doing alongside that in the community… He’s very engaged in so many ways and I have such a deep appreciation for watching, and listening, and learning, and watching his leadership in the things that he's doing here. This is a man that is fully engaged and fully committed to the issues of diversity, equity, and inclusion. With that I will ask you to join me as we call him to [inaudible 00:01:45] welcome to us.
[Lee Learman, Dean of the Virginia Tech Carilion School of Medicine]
It is very hard to follow NL Bishop making any introduction, and so I appreciate your very generous and kind words. I'm still a student of allyship, and I'm doing my best, and I'm learning every day, so thank you NL for that wonderful introduction. I just got to say that the person who brought us all here together today is none other than Ryan Bell and you'll hear from him in a minute.
It's been such a pleasure for me to work with Ryan since early 2021; I think it was, when he launched the Black Father Family Initiative and invited me to serve on the Steering Committee. For that I'm very grateful to have been asked and it's been a real pleasure and honor to work with you. Through the strength of Ryan's leadership and with the support of our partners at United Way of Roanoke Valley, the Black Father Family Initiative has grown in its scope, in its vision, in its strategy, and in it's programming in a very short period of time during a pandemic. It's been wonderful to be part of and to watch Ryan and his leadership.
When he shared the thoughts about tonight's program with me, I was immediately excited by the opportunity that this created for the greater Roanoke community and for our VTC community to all learn together from these wonderful guests and panel that we have tonight. It is a great honor for us to serve as the title sponsor for tonight's event and host in our building a conversation between Dr. Reverend Bill Lee; Founding Chairman of New Horizons Healthcare, and Dr. Robert Winn; Director of the Massey Cancer Center at VCU in Richmond.
Tonight, the attendees here in-person, you-all, and those who are viewing the live stream, we'll learn a lot about health disparities that affect black men, fathers and families, and the impact of these disparities across multiple generations. On behalf of the Virginia Tech Carilion School of Medicine and our faculty, staff, students and residents who care deeply about achieving equity in healthcare, we are grateful for this opportunity to learn more from this important conversation. Thank you very much.
[Video: Black Father Family Initiative]
My name is Ryan Bell and I'm the founder of Black Father Family.
Society paints black men as not being serious about the role of fatherhood, not cherishing the responsibility of fatherhood. I started Black Father Family to combat that narrative, to change that stereotype to begin to push against that stigma, and so we moved away from this idea of trying to combat a narrative and have shifted into this space of really taking on what the true concept of black fatherhood is. You can't beat what you can't see, and oftentimes we're not provided the opportunity to see black men enjoying their families and enjoying being dad. We take every opportunity that we can to expose and empower that image of a black man enjoying the responsibility of fatherhood. United Way Roanoke Valley's mission is to lift 10,000 families to self-sustainability. What better way to do that than through a father. The relationship between Black Father Family and United Way is one that is a perfect marriage of family stabilization with the role that fathers play within that family stabilization unit. Fathers are there emotionally. They need to be there economically, they need to be there educationally. They're there to advocate for their families and the communities that they live in. All of the things that the United Way is about. What better way to move the mission forward of the United Way and the mission of Black Father Family than doing it through the fathers that empower these families in these communities. For me, Black Father Family has become successful at the moment in the place in time where each father feels as though they are a better father to their children, they are a better father to their family, and whatever capacity that is for them at that particular point in time in their life. If they feel that they're able to be the individual who allows the opportunity for their family to move a little further along that journey to family stabilization, then Black Father Family has done what we need it to do.
[Ryan Bell, founder of the Black Father Family Initiative]
Well, good evening everybody.
[Audience]: Good evening.
[Ryan Bell]: First, I want to say thank you and I appreciate everyone who is here today and everyone who has decided to come and join us for this very timely and important conversation. The reason why I wanted to play that video first is to set the context for what the conversation is going to be about and why we're gathered here today. I want to take a few moments to dive a little deeper to set that context for why we're here today and why we're so excited about the work of Black Father Family moving forward. Today we're here for a conversation. We're here for a conversation on generational health, a conversation on black men and health disparity.
Recently Black Father Family just completed a new strategic planning process where we outlined what is it that Black Father Family is aiming to do and how do we do it? The key things in our new mission statement in Black Father Family Initiative creates a space for black fathers to find meaningful connections, support, and resources. The key in this and the key in the work that we're doing and the key that I hope we take away from this conversation tonight is this idea of creating community. How do we create community around black men? How do we create community around the institution that serves black men so that they can be in a better position not only for themselves, but for the families and the communities in which they reside. We do this for one particular reason; is to promote the health and well-being and the success of the children, families, and communities that the fathers are a part of. The work that we're doing with fathers is not really just for the dads, it's not really just for the fathers, but it's for the community as a whole. It's for the children that are in those families. It's for the units that surround those families. How do we position the fathers to be the most successful for themselves and for those around them? Now then vision.
Unapologetically, Black Father Family is about the work of black people. How do we position thriving black children, thriving black families, and thriving black communities? That is the vision of Black Father Family. We do that through the work of the father. Now, why? Why did we do this? Why is this important? Why is this a vital piece of the puzzle? The word is legacy. There's a quote I've just recently heard where it says legacy is not something that you leave for people, but rather something that you leave in people. That is what we're here to do with Black Father Family. We're here to position fathers to deposit pieces of legacy along their journey. Today, we're going to have a beautiful conversation about the legacy of health and well-being. How are we positioning fathers to leave a legacy of health and well-being for their children, for their families, and for their community?
[Ryan Bell]: Now I promise I wouldn't be it for you guys y'all. You guys are not here to hear me tonight, but I want to introduce to you guys the individuals who are going to be leading our conversation here tonight and then we're going to jump right into our conversation. When this idea first came about and we were having the conversation about health and well-being, who would be the perfect individuals to take part in this conversation? There was nobody else that I could take up to moderate this particular conversation, other than the Reverend Dr. William Lee. Reverend Dr. William Lee is the founding chair of New Horizons Healthcare. I recently just watched an interview that he did when he told the story about how New Horizons or the idea of New Horizons came to being. Correct me if I'm wrong. But it was this idea, this concept his father got sick.
His father became ill and his father did not have the insurance to take advantage of some of the things that he would have otherwise. New Horizons Healthcare is sitting here in my eyes, in my estimation just for community, just for family, just for children but of a son's desire to assist and help his father. That is the work of Black Father Family. Those are the seeds, those are the metrics that we're depositing in there. I couldn't think of anybody better than Reverend Dr. William Lee to come be a part of this conversation. He's a Former Pastor for Loudoun Avenue Christian Church for 39 years. He is the Founding Chairman of New Horizons Healthcare here and is somebody who I value and cherish very much in my own personal work, and so would you please help me in welcoming Dr. Lee.
[Ryan Bell]: Then we say, well, who can Dr. Lee have this conversation with? Who is somebody that we can bring in to have this conversation who we'll be able to learn from to maybe deposit some nuggets of wisdom in us on this particularly? I started scouring. I started looking at data and I came across the Harrison Museum's Lecture Series where there was a particular gentleman there who gave a talk and he just kept it real and honest. There was a level of vulnerability, a level of truth within that particular conversation and so we decided that that's what was needed. We decided that truth, honesty, and determination is what was needed for this particular conversation. We've reached out to Dr. Robert Winn. Dr. Robert Winn is what I'm learning very quickly was a rock star in the space of healthcare. He is the current director of the VCU Massey Cancer Center and is at a particular time of his appointment, was the first and only black to be a director of a National Cancer Institute-designated Cancer Center. Again, we're talking about legacy. One of the things that sold me on inviting Dr. Winn that really can't be a part of this conversation because I watched an interview that he did when he talked about this concept and during our time here today is repeated many times about the idea of taking science to the community, about taking health care to the community, about allowing the community to inform the work that we do. Black Father Family is in the position of positioning yourself and not tell individuals what they need and how it shows up, but how are we working with them to inform the work that we're doing. He is the epitome of that happening right now at the VCU Massey Center. We couldn't think of anybody else in bringing here to have this conversation with Dr. Lee other than Dr. Winn so please join me in welcoming our special guest.
[DR. LEE] Well, Dr. Winn, you and me. Tonight you'll get a chance to do something that the old folk and the black community would tell young people you're not supposed to do and that signify. But tonight you'll get a chance to do some signifying, and it'll be all right. This should be a private conversation between two colleagues, but we thought you all might want to hear what we had talk about so stick your nose and ears on end, then we'll have a good time.
[DR. LEE]: Dr. Winn, let me just get right at a piece. The literature that I reviewed states that black men suffer the worst health than any ethnic racial group in America. Why is it that black men have that distinction?
[DR. WINN]: I'm glad you asked that and before I get to that, I just want to be clear that the term health disparity is going to come up a couple of times a night. Before I jump into that, I want to explain to you what I mean by health disparities. We talked about differences in health outcomes. You can talk about African-American women with breast cancer versus white women. African-American women have a worse health outcome. When we talk about equity because many of us have now gotten into this hashtag, equity conversation. But I'm gonna be straight up. Equity is more of a dream and an aspiration. It is a principle that says that if we follow it, we should therefore be able to eradicate any health outcomes. But William, let's talk about health disparities. For me, for real, health disparities is rooted in social justice in the following way. Prostate cancer, we know in the United States that there'll be more African-American men dying from prostate cancer than white. Hold on. Except in the VA. What did we say? We talk sometimes about how in my brown skin I am more predisposed to disease by my biology. Unfortunately, we're not taken into a context the structure.
So disparities for me is the following. If you look at African-American and white men in a VA system, there is no difference in health outcomes from prostate cancer. Stop talking to me about that because I'm brown and because I'm black, therefore, I am just more biologically predisposed without understanding the history, without understanding the stresses that go with that, without understanding, we won't get down to it, not only the red line but the urban renewal project that ultimately build white roads through black bedrooms. Not only expose those neighborhoods to more toxins but by the way, there was a double shot of putting in businesses that weren't always great with the air. So when I talk about the differences of African-American men, I am reminding people, this is a complicated situation and it's not just my DNA that you have to account for is also my ZNA. That is my Zip code Neighborhood of Association. That's where we're actually taking the new science to so I know it's a complicated answer, but I just wanted to make sure that disparities rooted for me is in the context of social justice because if we were to provide the same things the VA does for everyone else, that means we should be able to close the gap, not because of my biology, but because of the structure.
[DR. LEE]: Well, since you just open the door wide.
[DR WINN]: [inaudible 00:17:17] That way you don't get invited back.
[DR. LEE]: Why don't you just go and dig a little bit deeper with that so that.
[DR. WINN]: I had done a little bit of work and it has been the most fascinating thing since I've come here now. I'm coming from Shytown, Westside by the way. But I know hate from my south side, brothers and sisters. Just say Westside. That's the way we roll. When I've come to Virginia, I've recognized a couple of things. I'll use Richmond as an example, but we can use Roanoke as well. In Richmond, there was an area called the Jackson ward. It was considered the Harlem, or the Black Wall Street in that area. The fun part about that area is that it's interesting because when I look at red lining, let's talk about red lining. Red lining was by Homer Hoyt who was a Wisconsin graduate, also developed for the FDA in 1930s the concept of redline. Now, where did that come from? It came from the soft science, call it what it is, of eugenics. It turns out that there was this crazy thinking that to pay back your loans, there was this sort of thing. We didn't had neighborhoods that were some what desirable and some were not desirable, and the desired and the non-desirable ones didn't get loans. That was called redline. But if you look at the red lining issue, I know people are starting to talk about redlining. We had our own banks, had our own commerce. Many of these neighborhoods actually, despite the redline and we're like, okay we good. But it was the issue of the 1950s and the '60s when we were talking about the urban renewal, aka slummer [inaudible 00:19:04] , where we literally divided communities that were robust and active, and cut them off. Many of these communities have never actually come back from that. I've been reminding my basic science colleagues, my translational science colleagues: quit talking about me and my predisposition of prostate cancer and why don't you add a little bit of the biology in addition to the genome? Why don't you add a little bit to that zenome talk about the history and the structures that have created us to have lack of access to care, but also environmental issues that also increase these things? That I think is the new conversation for today.
[DR. LEE]: Well, so let's stay here for a minute. Historically, given the Tuskegee piece and later years, Henrietta Lacks, on and on. Let's talk about why the racism and all of that just impacts this downward spiral with health of black men in particular.
[DR. WINN]: I love that question. You know what? Here's what happened on COVID. When COVID first began and when we started putting together these tests and all the rest of stuff, we started looking at African-American community saying, I don't understand why they're not getting these tests. I don't understand why they're not getting the vaccine. I always say that was well meaning, but when you take that and not understand that my grandmother, who by the way is from Remley, Virginia, actually would tell me not to go. I thought she was crazy. She would say, I don't want you to going to no hospital at 10 o'clock. Don't be going around them hospitals at 10 o'clock. They're going to take you. I'm like, man, she crazy. It turns out though that Dr. Uti and others have been writing this whole story about how black bodies were commercialized, grave robbing and all the rest of that stuff for the cadavers to actually do things on. When I say to people and they say, well, they're a little suspect, they're suspicious, you'd be crazy not to be. However, facts do have to play a role. Now look, I can't lie about your numbers. You can get to Dr. TikTok all you want to, but Dr. TikTok also told you that African-Americans couldn't get COVID at the very beginning of COVID and ultimately, it took us only a couple of weeks to be like, I think Dr. TikTok, you might be wrong on this one.
I think we are in a struggle now because we definitely have a reason to be rational. It would be irrational, I think for most African-Americans, including myself, not to be at least at a mumble like hold on now, but just because you are suspect and suspicions, doesn't mean that goes into following blindly to what I call the abyss of stupidity in the context of seeing right before your eyes that in 1971, 90 percent plus of the people with lung cancer died. Any women that actually had advanced breast cancer that you didn't have anything to do with. Since 1971-2022, not only do I have my chemotherapies, but I got a whole list. Look, when I was a medical student, I used to have to learn to talk. Back in the early '90s, I'd be like, well, we have a chemotherapy. Hey, Doc, well, give me the truth. How does it work? I'd be like, well, have you gone to Disney World yet?
In my lifetime, I've had a front row seat in seeing my patients go from giving them a drug that was called cisplatin-based drug or chemotherapy. Now I pull out. I'm like hold on, wait a minute. I got a immunotherapy drug right here. Hold on, wait a minute. I got to a molecular [inaudible 00:22:55]. Wait a minute. I know now that when you come in, even with advanced stage, I got something for you. It still remains that if most black men, we get checked early, you cut it out, it’s done. But the truth in the matter is this whole context of fatalism that we've had had for a while is some old news to me. I understand the United States Syphilis Study of 1932 and all this, I get it. I have it myself. Even though I learned how to wear a blue blazer, I'm from straight up the hood. When I get the other colleagues that doctor I be like okay, but the reality is if we don't have that trust, you'll get the double concussion. We'll get the concussion from the history of being paralyzed by not having the therapies. But the crazy part is, you also lose out again with our communities from not getting what I consider to be life saving in my lifetime can see it. I got women 15, 18 years, men, 10 years out from what would have been an advance, something that they should not even be walking not only just survive but thrive.
So for me, this is a testament of… Again, any wisdom I get comes from my father, my grandfather, John Don, and all the rest of them, but one of the things I was talking to brother Bill about a little earlier, I said we are in a time that we are stuck in almost a vacuum of pessimism and nihilism. The crazy thing is, to me, it is an insult and it is disrespectful to the legacy of the people who've come before us, who set the stage so that we might actually have some optimism and some hope to move forward. I'm going to tell you science, independent of what people say, has definitely moved forward.
[DR. LEE]: How do you get this science into the neighborhood, into the places where the science has not normally gotten?
[DR. WINN]: Now Dr. Lee, I'm going to get radical up in here and say some things that I know I can get a lot back, but you know what I'm saying.
[DR. LEE]: If you get any more radical, I'm heading for the door. Go ahead. We'll signify. Go ahead.
[DR. WINN]: Well, there you go. One of the ways is to be a little bit more thoughtful about exactly how do we get to communities. You don't get to communities by talking at them. Most health systems have taught at, not spoken with. In fact WB Yeats once said, I learned this when I was at Notre Dame back as an undergrad. I think once said, "Think like the wisest of men and women, but speak in the language of the people."
This disconnect that we feel between science is a relatively new sense of not belonging to someone because it means it's for those people. Big part of that has been access. If I were to actually have a magic wand, I would put much more money into our federally qualified health centers. I’d make sure that the federally qualified health centers are aligned and connected with health systems. By the way, that our community, instead of getting a health system navigator, why can't we get somebody from the neighborhood? When I was talking in the Westside, Chicago, someone said to me once, Doc, I got all what you say and he was smart dude man, but we just look for somebody to hold up a flag and say, here's where you park. But that's that whole concept of economic. That the economics of having connectedness to health systems from the neighborhoods is important. That's one. Two, we're going to have to train people differently. We just launched a national program. Man, I'm so proud about this. Clinical trials. Let me just quickly, when I say cool, I already see some people thought in my eye. I was listening it up to the top by some clinical trials, but hold on now. If you're a cancer patient and you've reached the end of the road with your standard of care, there ain't no other standard of care.
In oncology, what we do is we ultimately figure out there's a new drug X. Could it work? If it does work, then obviously it's going to take care of you right then and there. If it doesn't work, then ultimately we have given you not only standard of care plus. Not my data you can look it up. Most people in clinical trials, particularly African-Americans on clinical trials, tend to do better when they're on a clinical trial. Then when I just get the routine standard of care, not my data. Why? Because you get an exercise. We need to actually start thinking about how to embrace the future that is here. In fact, I say the future is here, it's just unevenly distributed. Our job is to getting back to your question, how do we realign those access to the most cutting-edge therapies that I know work? But how do we get them into African American… I'll start with this.
We know right now that we have more people in the United States right now, and probably my grandfather died from Alabama, Colon Alabama said, "When you're going to talk some, talk about somebody else, don't talk about them in their home now."
We're ain't going to talk more about Roanoke tonight. Not from me. It turns out that when you start looking at… Let's take lung cancer. One in two men will die from cancer. One in three women will die from cancer. It turns out that cancer, not cardiovascular disease is the number one killer of people in Virginia.
Most of you already know that.
Most of you also didn't know that when it comes to lung cancer, the people who die most from lung cancer?
African-American men.
The people who are dying mostly from pancreatic cancer?
African-American men.
We can go on to list but we won't. Why am I saying? I'm saying this? Because we know right now that if I had a African-American man come to me with lung cancer, the vast majority are not even biomarker tested. You'll still have doctors right now and says "You have advanced stage, and nothing we can do for you." Now, I started off the conversation saying "I got a whole tool kit now." Now, if you could get what's called genetic testing, I might say, "You have a biomarker. I got 3, 4 drugs for that." Most of us are still practicing 20th-Century medicine, even though we are living in the 21st century. If I had a magic wand, I would make sure that those things are available. That we are definitely aligning more with federally qualified health centers. I think that I'm back in the day FQHC guy. By the way, getting more communication that's out in the community about what we're doing and a more transparency could certainly help in last. I know it may not be popular, but you can't convince me that the lack of training and a lack of pathways for African-American men and others from our communities into these fields of science, that's a negative, not a positive. We need to figure out ways of how to make it. I love hip hop, and many of you know because I'm wearing a blue blazer real tight. But before I was wearing a blue blazer, I used to do things like produce some things for people like most of all though, people like Ryan Bell, he's little too young to know more his stuff is. Man I didn't even know who blocked us from the roof top but I was actually activated and motivate of understanding that my love for science, and my love for these things in part was just my passion, creativity. In fact, it was my grandfather who said, "When you go to college, you may learn nothing new. You just learn how to put tags on it. Namely, that's all you learn." For me, I think it's been a wonderful example of how we already have these infrastructures in place. We just need to align them better.
[DR. LEE]: You have started on my question number 6. Because literature states that black men and black persons in general, do better with their health if they have a provider who looks like them. The issue is all the four percent of the people who wear the white coat look like us. You've already just scratched it. Let's go a little bit deeper. As you're saying that there is creative genius that we're not tapping, that'll get our young people, they can do chemistry, they can do biology, they can do math if we find a different way to teach them. Help us get a room full of young black people ready to become our providers in the next 20 years.
[DR. WINN]: I'll start off by saying the following. I'll definitely love a beat. But if loving science is wrong, I don't want to be right. I will tell you that the love for science has been the following for me: That when we think about science, we tend to think of it as the other. We don't recognize that we have a very long history from Charles Drew and many other people. Lee Green who have been in the forefront and many people's names, you don't even know who've created the numerical drugs that we actually have. The sister that actually came up with the mRNA Vaccine is in North Carolina. When I talk about things belonging, the reality is, we have seen, I think sadly since the '80s, an erosion of some of these federal programs that to be quite honest with you, were working.
I'm going to be honest with you that I'm a walking poster child for many of these federal governments. I was born to a teenage mom. I'm a proud head start kid, everywhere I go, I ain't ashamed. I'm a proud head start kid. I had programs that then allowed me to actually get my first glimpse in the research at places like Roswell Park and other places in Cornell up in New York. I wind up having my first minority supplement award from the National Institute of Health. That allowed me, again, to break down this false barrier of us saying, "Science, that ain't for me." The reality is, if you think about creativity, it's the one place where you just get to create and think. I used to tell somebody that, is cool making some tracks and all the rest of that stuff, but you can actually have a whole entire career. You don't have to always run the lab. You can assist with running the lab and still make six figures.
By just thinking, how could I do good? I think I heard Russell Simmons once say to somebody, "Don't just do a job, what's the problem you want to solve?" The problem we want to solve in my neighborhood happens to do with, how do we treat cancer better? How do I take care of my grandma and my granddad in a hypertension? How are you going to solve that question? It ain't going to be just from thinking about it, you need to jump up in there.
I think what we need to do is get back to what was working. By the way, many of the programs that we're putting a place in the latter part of the '60s and '70s, we saw a flourishing of programs and a flourishing of numbers of African-American doctors and things like that and scientists.
The reality is we have to go back on this thing. Go back and figure out, what are those pathways? Those pathways shouldn't just be from the people who have access to everything. But a kid like me who didn't have access to everything, in fact, somebody said, "You must have been reading books since you were small." "No, the first book I read was on my own for fun was after I got out of college." Because I was like, "People read books for fun? I'll check that out." I do think as a culture, getting us back to reading, getting us back to talking to one another, and getting more exposure, because the crazy thing is, I don't think anybody knew that in 2019, when I accepted this job, I was the only African-American Cancer Center director.
Now, what's an NCI designated cancer center? I will just talk about that real quick. There are 6,000 cancer centers over the United States. But only 71 have been deputized by the federal government as being the centers of excellence. You have two in Virginia. I heard somebody once said, "If I get sick, I'm just going to throw my hands to the Lord." That's one way of doing it.
But you have two centers that have been designated by the federal government as being the best of. By the way, we even when you walk into my Massey, you're walking into 70 other cancer centers around the country. I call the people from Harvard, Dr. Glimcher, hey, give me a hand with this. What I think it is, is that we have an oasis, but we have been so fragmented and we have been so decentralized in our educational process within bringing our communities together. We used to just talk about this stuff in my barbershop. I had a Mr. Woods who was saying, I love what you're doing. They used to talk about these pathway programs in a barbershop. Many of those things have gone away. Additional federal support for some of those things, but local awareness of those things is what we're going to have to get back to.
[DR. LEE]: I've got three questions and then we'll have some opportunity to let the audience to throw some stuff at us. One question in particular. Again, literature says this, that black men have this thing called Black masculinity. That even when black males have the best insurance going, they are not likely to see provider for years. What is this black masculinity that will cause us to have an early grave as opposed to take care of ourselves, empower ourselves. We have systems that are hurting us. We're hurting ourselves also.
[DR. WINN]: I said to someone back in the day “when Mike Tyson was at his best would you just walk up in the ring and just fight that guy?” But that's what we do every day. By not getting us a fighting chance to having a prostate exams because we worried about, the funniest part, people say, well, “I'm worried about your finger.” Man, you've got a whole lot of things to worry about than somebody's finger. Come on now. That's going to be your test, that's why you not going to go? Or the other day someone said to me, well, you know, what if they tell me bad news? I told one brother once, I said, if they tell you bad news, here's the difference between telling you bad news early, and telling you bad news late is that when they tell you bad news and it's early, I can fix that. You can have maybe 20, 30, 40, 50 more years to just do your business. But when you come in and every piece of your organ is actually now gone because you just decided to rough it up and tough it up. This whole thing about keeping quiet and not talking. You know what the funny part about most of us African-American men is? I have now at thanksgiving once a year now, have made all men and my family and women, we talk about our health because I said, what's killing African-Americans is family secrets about our health. Now they would talk about the cousin some had. You know when you have breast cancer, but we can talk about no breast cancer now. Now look, the breast cancer, prostate cancer might be actually applicable to me because it may be genetic. I think that we are going to have to adopt much more of that it doesn't say anything about your masculinity to actually illustrate something about our intelligence. The intelligent man says, “hey man, if I got a little spot and I could take care of that, I got 50 more years.” But trying to actually just tough through it doesn't even make sense anymore. What I'm hoping to do is to start these crucial conversations of what you all are doing here in Roanoke, which I really appreciate. How do we just have more freedom to find courage? Now, I'll end with this. Most dudes can show physical courage. But the courage that is actually the most and the strongest is the spiritual and intestinal fortitude to make yourself vulnerable. There is not a courageous act. I'll put money on the table, not like the bank because we're going to be there. But I will say the following, you can't name a courageous act, not one, without having somebody be vulnerable. The baby carriage has gone down the hill that you then suddenly jump out and you see a car that's coming and you jump out and you try to push the baby carriage out, by definition simply means that you have made yourself now vulnerable and you've put yourself at risk. Most of the men, particularly African-American men that I'll meet these days, even one's got the popcorn muscle, acting manly and all that tough. Did you go get your digital rectal exam? I didn't get that. Well, you ain't all that tough. I'm trying to become it up, trying to front it like that. You clearly aren't all that tough. I think we have to re-frame what it is that we think about toughness, and toughness, the physical toughness is one aspect of toughness. But the real toughness comes from doing those things that you make yourself vulnerable and find that courage within that and that's spiritual courage. Then intestinal fortitude to do those right things. Not only just for you but your family and everybody else. That's real courage and I think that message, we should get out more.
[DR. LEE]: Two other questions. You and I have connected on this down for at least last three years. During COVID, you align with Reverent Todd Gray of 5th Street Baptist Church and others, had what was called Faith and Facts Friday. You were trying to help the black community to see, you were bringing science into faith and said the two can work together. What I'd like you to talk to the audience about is the connection of faith and science, but especially how the black church can be what I call in my work a portal of health care. I think it's a key place where black people, especially black men may indeed find an intro into the health world.
[DR. WINN]: I agree. I have, on some Sundays told somebody, now look, you all act like black folk. We don't do no science. I go well, you read the Bible? I read the Bible. I read my Bible every day. I go, you read the thing in Daniel? You know where your Daniel Diet comes around? You know what a Daniel Diet? The Daniel Diet was science, it was, how do we go back to ultimately figure out? I said, quit. Don't be playing with me with all these hick-yackety stuff that you don't know science. The first thing is, for me, Martin Luther King, I think said it best. Said the four pillars, when you came to the pillars of the African-American community, you had the press, you had the fraternities, of top number one was the church. In fact, you all remember back to early 2020, when COVID was coming out. Who would you believe? Sometimes the information coming out right from the CDC was mixed. People weren't believing scientists. They certainly weren't believing doctors. By the time where I actually had to come up with you and when we talked about the vaccine, people like, you trying to give us and kill us off? I was like, now look. It turned out that it was a moment of clarity that if we will go and get the voices out, we need to get the voices to the most trusted.
We had real crucial conversations in the beginning about COVID. Towards the end of May 2020, we launched the Facts and Faith Friday because we thought that facts are not at war with your faith. No need for facts or faith to be at war. In fact, it was the central part of that, that got multiple black churches together. That then said, not only how do we disseminate information to our congregation, but what I loved about these men and women from these faith-based leaders is that they were committed to the community. It wasn't enough just to say, we got to get this information out to all the people coming to church, but how do I get the information out to our communities? In fact, they were probably some of the best carrots. In fact, I have to laugh because some of them would say, well, why don't you join? I would say, look, how often do you get someone from the CDC? You know who we got? Christa-Marie Singleton, African-American woman who actually stayed even doing an administration because she said she is not going to let nobody run her away. Best part is, she got on, she got on the Zoom, I was like, you know you work for the CDC, you can't say this.
She goes, well, first of all, I want your pastors and everyone know, they ain't nobody going to run me away for what I worked so hard for and she goes “I'll always tell you the truth even if it means my job. That's what I'm here to do.” And so imagine now having cutting edge information, not from somebody who knew cousin Ronnie who heard it on Google, but someone right from the CDC that you can even ask the question. The best questions she ever got to ask is, why you all look confused? She said because we are.
Again, so just so you all know, we don't record it in so, I had to see, I'm recording none, no, it's this in a moment. But having that real transparent conversation and having it actually, so people say so what? You had these conversations. You can look at every one of those parishioners and those faith-based leaders as part of Facts Faith, their churches wound up with probably fewer people getting COVID. In fact, I credit them with saving thousands and thousands lives. They are like Dr. Winn you did, I'm like no. Faith-based leaders who had these conversations saved thousands and thousands of lives. In fact, are now part of the solution of how we get back to churches. But if you look at most of those churches, the uptick in vaccines and all these other things was directly related to that Facts and Faith Friday and those faith-based leaders. I have nothing but mad respect for the Black Church.
[DR. LEE]: Well, thank you. Since we are sitting in this marvelous building, this medical school. I just thought I would throw this out. What you just said, says to me, that there needs to be an intentionality between medicine and especially Black church. Tell me, help us find out a way that before there's a crisis, before there's an epidemic, are there educational pieces, are there lectures, are there seminars that we could be ongoing so that when the trouble comes, we already have built a trust-base?
[DR. WINN]: Yeah and that's a great question. I'm going to steal this one from my aunty. She used to say to people, "You know what, you need to connect with me before there is a crisis." I think in that vein, having programs that actually have health systems, not when you're in a crisis, but having regular cadence of communications and openness is important. This Facts Faith on Friday turns out that it's one of the few programs that even as COVID is, we're getting through COVID. Many of the other ones have died down, we now are talking about issues on mental behavioral health, particularly within the black community, which again, is a taboo subject. Because apparently some of us feel like everybody else except for black people get depressed. I wish that were true, it is so not true. We are starting to have these issues around policing and all the rest of these other conversations and so we've opened up what was initially a weekly conversation around COVID to now talking about screening for cancer, we're talking about other issues, about housing, we're talking about transportation issues. But the point for me was that it's now become a venue that everyone looks towards because it's now like cohort of people that get together and conversate, as opposed to there is now something happening in African-American community where you see a crisis, and now all of the sudden I want to step in, to your point. I do think that my aunt was right, if you want to really connect with me, connect with me before there's a crisis. I think we have to have more of these touch points about conversations.
[DR. LEE]: My last question is, and because you have said it over and over again and throughout dinner. Well, what I rediscovered that you cut your medical teeth in a federal qualified health center in Chicago. Talk to us a little bit about how you see FQHC's helping us with these health disparities and making a better health pathway. Not just for black people in this case, but for people who are poor, the socioeconomic low end spectrum?
[DR. WINN]: You know what? I think of the history of community health centers starting all the way from 1942 with Dr. Clark. I think of Dr. Hatches from Mississippi and Dr. Geiger setting up something here in the United States that was literally meant to be the undergirding. The war on poverty, part of that was to actually, back in the day, remember, they would write scripts for food. I learned that. As we start thinking about things like federally qualified health center, we have the undergirding infrastructures to really work with. I actually think that the next level is how do we bring more? How do we bring more resources? I was just telling you a little bit earlier that when I was at an FQHC, I did one thing. I was trying to bring science more to the FQHC. On the south side of Chicago, this is where Bernie Mac comes from. Dee Rose, Englewood is Englewood. I had a town meeting like this on the 16th ward. One of the Alderman bought us there. I had a group of guys. Well-meaning, so don't take this like I'm slamming my people because they are my people, I brought them. Three of my top scientists because they said I want to go. I said, well, are you want to go up to 16? Well, they said, I want to go. They started talking science talk. You can see mostly people, audience were nodding their head and understand what's going on. But they were like, yeah, okay. They were giving me that quiet nod. But oh my goodness. One of them actually did something that I was telling you that it was almost like a movie that if I could go back and be like, no. My man stepped up, they say, well, we know you scientifically, you all are scientifically illiterate, oh my God.
This 87 year old woman stood up and talked to somebody else. You see? She came up and she shuffled to the mic and she said, "No, what are you saying again?" She said, "Well, we might be scientifically illiterate, but you're illiterate too." That was a lesson for all of us at that moment, that there is stuff to be learned in the community. There is stuff with any FQHCs that can be taught so that we can inform what we believe are the places that have all the information. They don't. This is where we talk about bench to bedside. This is whole 1950 miles out, I come up things in my laboratory that I get it to my bedside and we do clinical trials on you and then we make you better. Well, I got something. How about people to a pipette or community to bench, where we're informing the scientists on how to refine their scientific question. That's what we're trying to do now.
[DR. LEE]: Thank you.
[DR. WINN]: Oh, no, thank you.
Call for questions from the audience
[Ryan Bell]: We have two mics up here in the front. If anybody has questions, just come approach the mic and ask your questions. Ask away.
[DR. WINN]: Thank you all for putting up with me tonight. I appreciate you.
[DR LEE]: Ryan. Just for logistics, we stop at 8:30?
Yes. I just want to make sure folks will give a dissertation, but their question. You got to hit them hard. Let's go.
Say.
[AUDIENCE MEMBER ROB YB YOUNGBLOOD]
Yeah, you shouldn't have said that I'm alpha male. We tend to be very long-winded. Excuse me. You said we was in church, so we're going to tell [inaudible 00:51:48] the devil. Peace and blessings. My name is Rob "YB" Youngblood. I serve as the chief, a connecting officer at YBConnects and are proud to be a partial sponsor to this event. As a connector, you talked about the importance of organizations and churches getting together. What can I do as a connector, what can connectors do to be able to bring these organizations together, the fraternities, to be able to deliver these messages out so that we can educate more people in a rapid fashion?
[DR. WINN]: Yeah, that's a great question and I'll keep it brief by saying that I think right now is the age of knowledge. We say it's the age of technology, it's the age of all social media. But I'm surprised at how little people still know. The reality is while we have high-tech, I think to your point in the context of connected, we're going to still require high touch. From my perspective, you're connecting again pieces of what we're doing tonight. If you wanted to know one of the baddest people in the United States right now doing genetic medicine, his name would be John Condon, a brother from Crenshaw. I mean, his brother, not Crenshaw. I mean, his brothers from Crenshaw. He actually has been doing wonderful work. We have now created believe it or not over the last 30-40 years, a number of amazingly talented people that the issue is we just don't know how to dial in. The connecting would be how do we continue this conversation? Now that make this a one and done. Just quickly by the way, one of the things we've done this in and for young people is, I don't know if some of you all probably know common, and some of you all probably heard of saying, what's is his name? Kanye West. 1.0 I'm talking.
I'm just letting you all know for the record over here. There was a producer for him that laid down the tracks a young brother named Timbuktu, some of you may know him. He died of renal cell carcinoma, I think in his late '20s, his name is Timothy Francis Jones, going to connection. They reached out to me and said, what can we do to bring about more information so that young African-American men and young people get a better grip on reality is that they don't have to suffer. I tell Timothy Francis Jones Timbuktu's story because at the same time, the head of what's called the Precision Medicine Initiative, of which I was a part of back in 2015 when Obama was there, was saved by Precision Medicine. A young white man at the time because he had access to the cutting edge science that came about from what we were doing, and so much so that he was then able to lead the program at the NIH. I tell you the story because once a year we get together and we have everybody from Ghostface to red alert to all my folk about west. You have all the Hip Hop house artists. They literally get together for free, they fly in just to do a whole show to raise money. But more importantly to start raising awareness. The young people, that it's actually okay to talk about the fact that one in two men will die from cancer, one in three women will die from cancer. When you start looking at the African-American community that one in two is number one leading. Through music and through other activities, we're now trying different angles because, a brother may not actually want to hear it, I ain't going to have no cancer. Well, it turns out that young folk with leukemias, lymphomas, the funny part about cancer, cancer just don't seem to care. You can be republican, democrat, you could be like, [inaudible 00:55:30] 24 ways, you could be whatever. Cancer does not care. When it happens, we want to be there to say we understand because culturally as African-American men, we are not wired for some reason at least that’s the myth that they tell us, we're not wired for health, but that's actually not true. We just have to actually be essentially exercise that muscle. That's what I think you guys are doing really well here in Roanoke that I want to pattern after with your program, with Ryan, what you guys are doing, and Dr. Lee what you guys are doing, with your FQHCs and other things, you guys are laying the stage for how we can do things differently and when they reconnect us.
[AUDIENCE MEMBER DANIEL BROOKS]
Dr. Winn, Dr. Lee, I appreciate this conversation, Dr. Bell, Ryan, thank you for this opportunity to be here. My name is Daniel Brooks, I'm a local licensed clinical social worker who created these mental health initiatives to do the same thing that you're able to do and spread this word and our mission statement through our companies making healing possible. But my question is how can we do a better job of merging the worlds of healthcare, physical health care and mental health? Because what we see is, we were talking about with this sense of black masculinity. That's a mental health barrier. The thoughts of where did it come from, why do you feel that way? Why do you think that way? That drives home some of these mental health issues that a lot of our black men aren't dealing with, which in turn makes them not want to go to seek help. Then the last part of that question with merging them because most of the time it appears in my journey walking through the mental health world is that as mental health workers were seen lower on the totem pole than physical health workers. How can we be on the same level in order to push this thing forward, to be able to help this holistic view for black men and individuals?
[DR. WINN]: I appreciate that question for real, for real. Let me start out by saying something that my grandmother, I thought was a quote until I did the work. I found that it was from Theodore Roosevelt, but it still works for me. She would always tell me, "People don't care how much you know, until they know that you care." I don’t think our health system, just being fair, has always talked about how much we care. We've been about the business of telling you how great we are, how we're coming up with the next cure. How we are the most wonderful and our scientists are the most dominant in the world, so much so that that language has disconnected us. Going back to your original question, from knowing that the health systems are really built on a foundation of having people know that they care. Part of this is going to know that they care, which is going to tie back into the second, I'm going to keep this short. Is clear that you can clearly have a physical body that is well. But we've seen mental health in front of us and what it does. Now, for some of us, we saw when Mike Tyson wasn't well, we've seen Dennis Rodman. Now, this again taboo subjects we will be like, don't be talking about that around, you know what I'm saying? We understand that just because you’re physically healthy, we understand the impact of the mental issues. If it hasn't done anything else, COVID's brought that to light that you need, both mental, physical and I'm going to throw in another one, spiritual health. I think we are now much more aware than we would have been in 2018.
In 2017, we blow that off, and what you're going to hear is a lot more conversations around the interplay between that mental health and the physical health. Thank you for bringing that message up. But again, I think my grandmother was right. The system people say, well, why don't more black folks trust the system? Because it's not obvious that the system actually cares. This is where communication and language is actually going to play a critical role as much as the next molecular innovative drug, the next phase of the 21st century of how are we going to turn the ship around, is thinking about the science of communication and actually understanding the humility and grace, as my grandma would say, is that we're here to do a job to serve.
[AUDIENCE MEMBER LINDA MAYANS]
Good evening. Thank you. Dr. Winn and Dr. Lee, appreciate it you letting us being on your conversation. My name is Linda Mayans. I'm a retired registered nurse from the VA Medical Center here in Salem, Virginia. I've been on webinars with you and I always said if I got the opportunity to be in the room with you, I need to ask you some questions. I realize this is for the men, and all the things I had to ask about men, you've already answered them about the disparity, the reluctancy, why they don't go and get their prostate exam and everything. But I need to ask you something about the women because you are at the Massey Center in Richmond, one of the head areas that we can get services from. My job is encouraging women, particularly young women, any women, early detection is what you need to do. I know you talked about clinical trials and I know they are different.
Science has come a long way. When I first started back in the 70s working on a cancer unit, people just died. They just came, they slept, they died. We didn't even give them pain medication because we felt that they were going to get addicted to it. Science is not where it was 40 years ago. But there are things coming up. I'm recognizing now a lot of our African-American women, just not African-American women, the diagnosis they get is triple-negative cancer and there's not a targeted therapy for that treatment. Are there any trials being done in that area and how are we looking as far as helping our African-American women?
[DR. WINN] Thank you for that. I'm going to say it this way, my grandmother and she now all 96 but she's sharp as all get out.. She had a song she used to sing when she ran the kitchen, look how far we've come. Bought us out of darkness into the marvelous light. Look how far we've come. The reality is I've had a front row seat of understanding how far we've come, certainly in science, triple-negative breast cancer turns out I'm going to hit you with something else and I'm a leave this alone because trials are underway. But let me hit you with this. Turns out, that we go around talking about black, what did you say? About black folk. Now look here, Lisa Newman from New York has shown what we're not talking about though is ancestry and I'm going to hit this up in two seconds, I swear. But look here, it turns out that if you are in Roanoke right now, and I'm taking this audience and you come in black, but it turns out you have triple-negative breast cancer, now hold on with this one, and it turns out your ancestry says that you are more of East African descent. You will have a better outcome than your triple-negative breast cancer, what did you say? Hold on now, it goes even deeper, if you're a man with prostate cancer, it turns out, hold on, that just being black ain't enough. If you are black person male with more what we would call western ancestry, you will have a worse outcome of your prostate cancer. When I talked about zip code, neighborhood of association, I wasn't playing, it's about place and space. What we're not doing is the real PSA in a context of not only these precision medicine and service, but ancestry. How many people, as we are actually taking care of you, we talk about the promise of precision medicine, but it's a hashtag. The real issue is what we're going to be trying to do at Massey is not only understanding your blackness or understanding your whiteness, because it turns out that if you are from Eastern Europe as opposed to some parts of Western Europe, the same thing applies. Let's stop playing, science should be moving us forward and a science just say that black is just the start. We need to actually start using the tools we have. Because I now have had several women that I've actually referred back up to my friend Dr. Lisa Newman of Eastern African descent, I said run the ancestral pattern. She ran ancestral pattern and it turns out that they were more East African than West African and guess what, we started tailoring our therapies and having better outcomes. I just want you all to be awakened to the fact that when we say black, there's a whole lot that goes into there. Not all of us come from Ghana, they were different parts of the diaspora that we arrived here from with certain connections back to that diaspora if you like it or not. Now, people talk about DNA. Let me just hold on with you know, that's some of the diseases you got have been imprinted in your DNA from several generations of stress before. That used to be something my grandmother used to talk about, I swear to God. I wish my grandma was here because she said, "This boy, he didn't learn everything you know for me."
I swear to God. She used to walk around the house saying something I thought was crazy. She go now, "So and so got that disease because her great grandmother had it." You'll be like, "How does going to do with it?" It turns out, that the reason why folks like Serena Williams and Beyoncé, who have all the money in the world, have the difficult pregnancy wasn't simply because of their blackness but it was because of the ancestral DNA imprinting from those stresses in those genes. What I'm saying to you, why do I love science? Because science shouldn't alienate us. It should bring us closer to our creator. From my perspective the science is bringing me closer to the greatness of how things have been put together and it's our job to understand that so we can better help, whether you are from rural Beattyville, Kentucky or Danville or Roanoke or the east side of Richmond, I'm just saying. Just saying.
But there is this wonderful thing that's actually happening now that we're going to be pushing our health systems and providers into understanding, how does our ancestral markers, not my blackness, but the ancestral markers play, and not just for black people, it's for all. That's real precision medicine and that's where we are headed.
I'm starting to get all hyped up about that.
[inaudible 01:06:51 – unidentified audience member speaking off camera].
[DR. WINN] I love that.
Again, going back to my family, grace and humility. What happens is sometimes we are coming up with answers before we actually have it from the person we just asked. I've been in a number of rooms, by the way, where someone just assume that I was an expert on something and I was like no, what? I don't know that. What we're doing now, having open and honest conversations, is the first step to healing even our country. When I talk about being gripped by that nihilism and gripped by the pessimism, you can't have a conversation with someone that you don't know. That you can then build up trust with your neighbor and then have more difficult conversations. If I want to come in and actually talk about something really hard and I don't know you, I got my Westside Shytown and I'll be like, who sent you because I ain't talking to nobody who ain't sent you. I think that we're at a wonderful world of having a little bit of humility, of understanding how do we build, and I think we talked about it earlier, relationships. I'm now able to have conversations, I swear to God, with people who were COVID deniers. One of my chemotherapy told me that I was just trying to get them in poison. I won't say where they're from but I will say that they had a confederate flag but, unfortunately, I did some countries who is able to talk about a couple of country folk, Charley Pride and Lester Earl Flatt Scruggs and all of sudden we had a different conversation that led to him saying, well, you look like you're okay. That conversation of you look like you're okay was better than the medicine I gave. When we talk about what can we do, let's start having the grace and humility to do the simple things not solve the problem. Let's start building the relationships because that, to me, is our best hope for us. But I appreciate that question too. Hopefully when this happens I know you all are going to keep it tight. Now I'm his spy so I'm going do something like this will be rich, I am going to get everybody talking. But this talking now is probably more important now than ever before if we are going to save ourselves. By the way, when people talk about, well it ain't me, we got a term called body image agnosia. I'm going to show you what that looks like. If this is your hand but you don't see that it's your hand you're like, what the hell is that hand doing in front of me? He is all along everywhere I go, this hand's coming. I'm like, but that's your hand. This ain't my hand. That's attached to your body. This thing ain't attached to me.
That's body image agnosia. When we start talking about problems in our community and we say, well, that's not my problem, hold on. I'm just saying I'm going to leave it there. We're all in this together and if COVID didn't show us anything, it showed us that no matter where you are it's going to touch you. Remember that one in North Carolina we had a whole bunch of rich folk run up to Bald Head, North Carolina.
Did you all hear this story?
They took off, they went to Bald Head, North Carolina, bunch of rich people and say, "Where are we going to go and escape? Now, who was watering the grass and bringing the food?" It turned out that the whole Bald Head North Carolina and all 90 percent infected rate, were like, "How do we get out, come on, man?" Let's not pretend that we are not all in this together. When there is something sick within our community we are all dealing with that issue so I think having the humility and the awareness that it's our problem literally is actually going to hopefully be something that we can move ahead with and be successful. I know I've taken up too much time, I apologize, but thank you so much.
First I want to say thank you, Dr. Winn, thank you Dr. Lee so much. Can we give them one more round of applause.
Next, I would like to recognize a few people and organizations that made this event possible. First, I would like to recognize Mr. Robert Young Blood and YBConnects and VTC alumni relations as one of our sponsors. I recognize the John Brauer, he's in the position as CEO and presidentof the New Horizons Healthcare is one of our sponsors here tonight. Also I would like to recognize an organization that is near and dear to my heart and President Keith Lang of Alpha Phi Alpha Fraternity Incorporated as another one of our sponsors tonight, I believe he is here. That's him.
Of course, to our title sponsor to Dean Learman, thank you so much for making this possible, to the Virginia Tech Carilion School of Medicine for being such gracious host, not only of this event, but all of the events that have happened here this afternoon. Thank you so much. This couldn't have happened without you, so thank you. Certainly not least, thank you to each of you for coming out here and joining us here this afternoon to have this conversation. There's a few things I hope you'll take away from this. The last piece of what Dr. Winn shared is about relationships and we're all in this together. This work can't get done without everybody here in this room finding out where they fit in, how they fit in, having the conversations, and being willing to offer some grace and humility. The last thing I'll share with you to each and every black man in here who loves and enjoys being a father, thank you, I love you. Continue to keep doing what you're doing and be on the lookout for some great things coming from Black Father Family in the future. Thank you.
Please join the Virginia Tech Carilion School of Medicine for a conversation hosted by the Black Family Father Initiative between Robert Winn, M.D. and Dr. William L. Lee as they discuss the health disparities that affect black men, fathers and families in our communities.
Hosted by the Black Father Family
Sponsored by
- Virginia Tech Carilion School of Medicine
- New Horizons Healthcare
- Alpha Kappa Lambda Chapter of Alpha Phi Alpha Fraternity, Inc.

As director of VCU Massey Cancer Center, Winn oversees a cancer center designated by the National Cancer Institute that provides advanced cancer care, conducts groundbreaking research to discover new therapies for cancer, offers high-quality education and training, and engages with the community to make advancements in cancer treatment and prevention equally available to all. He is leading the nation in establishing a 21st-century model of equity for cancer science and care, in which the community is informing and partnering with Massey on its research to best address the cancer burden and disparities of those the cancer center serves, with a local focus but global impact. A pulmonologist, Winn is committed to community-engaged research centered on eliminating health disparities.

Lee is the founding Chairman of New Horizons Healthcare. The origins of New Horizons can be traced to active grassroots efforts initiated in the early 1990s to improve the health of the residents of NW Roanoke. Loudon Avenue Christian Church, where Rev. Lee served as pastor for 39 years, served as the first home of New Horizons Healthcare.
Statement about accessibility and accommodation
The Virginia Tech Carilion School of Medicine is committed to creating an inclusive and accessible event. All virtual events will have automated captions. Recorded events will have edited captions available soon after the event. If you desire live captioning or a sign language interpreter, please contact the organizer two weeks before the event.
For in-person events, the main VTCSOM building at Riverside 2 is wheelchair accessible from the elevators inside the parking garage. Blind or visually impaired users may need assistance finding the elevators under the building, or using the stairs in front of the building.
If you need a reasonable accommodation to attend an in-person event, please contact the organizer of the event. All reasonable accommodation requests should be made no less than 2 weeks before the event. We will attempt to fulfill requests made after this date but cannot guarantee they will be met.